That’s where I met Mayank — fit, cheerful, and in his 30s. Over cups of chai by the lakeside, our conversation took an unexpected turn.
“Tanuja, my ultrasound says I have fatty liver. I don’t drink, I’m healthy… Should I be worried?”
It’s a question I’ve heard so many times — quietly tucked behind casual health checkups, often brushed aside.
Under the open sky of Kashmir, that simple question reminded me: Fatty liver isn’t rare, but it is often misunderstood.
This blog post is for people like Mayank — and maybe, for you too — looking for clarity, facts, and peace of mind.
Introduction
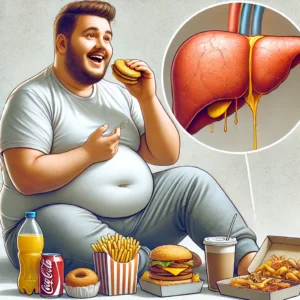
“Non-alcoholic fatty liver disease (NAFLD) is a silent epidemic, now affecting 1 in every 4 people globally — that’s nearly 25% of the world’s population.”In cities, the prevalence is significantly greater, particularly among women with PCOS and young professionals. In India, nonalcoholic fatty liver disease (NAFLD) has surpassed viral hepatitis as the primary cause of liver disease. Programs for national awareness are desperately needed. This group of liver diseases is distinguished by the buildup of hepatic fat (>5%) without a substantial alcohol intake. NAFLD can progress to non-alcoholic steatohepatitis (NASH), which can lead to cirrhosis, fibrosis, liver failure, and potentially hepatocellular carcinoma (HCC).
A recent article in the Times of India highlights the alarming rise in liver disease-related deaths, especially linked to lifestyle choices. Is your lifestyle harming your liver? – TOI, June 29, 2025
🎙️Podcast: Fatty Liver Disease

🧭 Natural History of NAFLD

NAFLD develops gradually and silently; it is not a static condition. Without treatment, it can progress from simple steatosis (fat accumulation) to MASH (inflammation + liver cell injury), cirrhosis, fibrosis, and in extreme situations, hepatocellular carcinoma (HCC). Early identification and consistent lifestyle modifications are essential to reversing or stopping the disease because of its gradual course, which can take years or even decades.
🩺 Screening Guidelines: Who Should Get Checked?
While not everyone requires a liver screening, some high-risk individuals shouldn’t wait. Those who have metabolic syndrome, PCOS, type 2 diabetes, obesity, high blood pressure, or dyslipidemia are among them. Liver imaging and metabolic tests are worth considering for anyone over 40 who is getting regular checkups. Irreversible liver damage can be avoided by detecting NAFLD early.
🩺 What Are Cardiometabolic Risk Factors?
Cardiometabolic risk factors are clinical and biochemical indicators that increase the likelihood of developing fatty liver diseases/ MASLD (Metabolic dysfunction–associated steatotic liver disease). Recognising these early can help guide lifestyle changes and prevent progression.
✅ Key Cardiometabolic Risk Factors and Cut-Off Levels:
| Risk Factor | Cut-Off Value |
|---|---|
| Body Mass Index (BMI) | ≥ 25 kg/m² |
| Waist Circumference | > 90 cm in men > 80 cm in women |
| Fasting Blood Glucose (FBS) | > 100 mg/dL |
| 2-Hour Postprandial Glucose | > 140 mg/dL |
| Haemoglobin A1c (Glycated Haemoglobin) | > 5.7% |
| Blood Pressure (BP) | ≥ 130/80 mmHg |
| Plasma Triglycerides | > 150 mg/dL |
| HDL Cholesterol (Good Cholesterol) | < 40 mg/dL in men < 50 mg/dL in women (optional, stricter) |
Compared to white Caucasians, Indians often have a larger percentage of body fat, with the majority of that fat being concentrated in the abdominal cavity. Because it affects metabolism, body composition—and fat distribution in particular—is significant. Hence, for the Indian population BMI >23 is taken as significant.
NAFLD is frequently associated with insulin resistance, dyslipidemia, type 2 diabetes mellitus, obesity, and metabolic syndrome. For prevention and management, early identification and lifestyle modification are essential because the illness is mainly asymptomatic in its early stages.
Nearly 80% of patients with Metabolic Syndrome have NAFLD
🧬 Why These Cut-Offs Matter:


These parameters help define whether a patient is at increased risk for metabolic liver disease or needs early intervention. Even one or two abnormal values may indicate underlying metabolic dysfunction.
To effectively manage and prevent NAFLD, we will examine its causes, symptoms, diagnostic tools, treatment options, self-care techniques, and lifestyle changes.
🧍♂️ NAFLD in Lean Individuals (Lean NAFLD)
Yes, having a fatty liver is possible even if you are slim. Due to nutritional and genetic factors, lean non-alcoholic fatty liver disease (NAFLD) is prevalent in many Asian communities. Despite having a normal BMI, these people frequently have visceral obesity, insulin resistance, or sedentary lives. Due to a lack of awareness, both patients and doctors must consider factors other than weight when determining liver risk.
🩺 What’s the New Name for Fatty Liver Disease ( Steatotic Liver Disease/ SLD)?

The medical world is moving away from the term “fatty liver” and now calls it Steatotic Liver Disease (SLD) — a less stigmatising, more accurate name.
Previously known as NAFLD (Non-Alcoholic Fatty Liver Disease), the updated term is now MASLD (Metabolic Dysfunction–Associated Steatotic Liver Disease), reflecting its strong link to lifestyle and metabolic health.
| Aspect | NAFLD | MASLD |
|---|---|---|
| Definition | Fat accumulation not caused by alcohol (≥5% hepatocytes). | Fat + ≥1 metabolic risk factor (e.g., diabetes, obesity). |
| Focus | Excludes alcohol and other causes. | Highlights metabolic dysfunction. |
| Terminology | “Non-alcoholic” label. | Cause-based positive label. |
| Population | Broad group defined by exclusions. | Refines based on metabolic risk. |
| Diagnosis | Steatosis + no alcohol intake. | Steatosis + ≥1 metabolic risk. |
🔍 Key Takeaway:
- MASLD ≠ is a brand-new disease — it reframes NAFLD to focus on metabolic dysfunction.
- The goal is better diagnosis, treatment, and awareness of the real root cause.
🧬 What is Metabolic dysfunction–associated steatohepatitis (MASH)?
MASH is the new medical term replacing NASH (Non-Alcoholic Steatohepatitis).
It describes a more severe form of fatty liver disease, where fat buildup in the liver is accompanied by inflammation and damage to liver cells.
This condition can silently progress to fibrosis, cirrhosis, or even liver failure if not addressed early.
| Aspect | NASH | MASH |
|---|---|---|
| Name Focus | Focuses on exclusion (non-alcoholic). | Focuses on metabolic dysfunction. |
| Definition | Fat + inflammation + ballooning injury. | Same but within MASLD when inflammation present. |
| Diagnosis | Traditionally by biopsy. | Histology or emerging non-invasive tools. |
| Meaning | Subgroup of NAFLD with risk of fibrosis. | Subgroup of MASLD with same risk. |
| Reason for Change | Exclusion terminology. | Cause-based clarity. |
MASH isn’t a new disease — it’s a smarter label that reflects why it’s happening.
🍷What is MetALD and How Is It Different from MASLD and ALD?
MetALD stands for Metabolic dysfunction and Alcohol-associated Steatotic Liver Disease.
It’s a new term under the broader category of SLD (Steatotic Liver Disease) that helps doctors better classify liver issues when both alcohol and metabolic risk factors are involved.
| Term | Meaning | Cause(s) | Key Difference |
|---|---|---|---|
| MASLD | Fat in liver due to metabolic issues | Low/no alcohol + metabolic dysfunction | Not alcohol-related |
| ALD | Fatty liver from alcohol | High alcohol use | Alcohol as main cause |
| MetALD | Mixed metabolic + alcohol | Both causes present | Overlap of MASLD and ALD |
*MetALD requires at least one cardiometabolic risk factor + moderate alcohol intake.

MetALD: Alcohol consumption 20–50 g/day in women and 30–60 g/day in men
Alcohol-related liver disease (ALD): Alcohol consumption >50 g/day in women and >60 g/day in men)
✅ Can MASLD Coexist with Other Liver Diseases?
| Condition | Can Coexist? | Remarks |
|---|---|---|
| Autoimmune Hepatitis | ✅ Yes | May affect treatment. |
| Viral Hepatitis (HBV/HCV) | ✅ Yes | Accelerates liver injury. |
| Genetic Liver Disease | ✅ Yes | Needs dual management. |
| Drug-Induced Injury | ✅ Yes | Important to distinguish damage. |
Causes of NAFLD
Although the precise aetiology of NAFLD is unknown, several variables have a role in its development. Insulin resistance is one of the key factors, and it doesn’t just affect blood sugar — it throws the entire metabolic system off balance. As fat builds up in the liver, cell function declines and inflammation rises, quietly laying the groundwork for NAFLD and NASH to develop and progress.:



🧬 NAFLD and the Gut Microbiome
According to recent research, the development of NAFLD is linked to gut dysbiosis, or microbial imbalance. Endotoxins may enter the liver through a leaky gut, causing inflammation. Diets heavy in prebiotic fibre (bananas, onions, and garlic) and maybe probiotics may improve gut health and lessen liver stress; however, research is still in its early stages. Before beginning to use supplements, always get your doctor’s approval.
Symptoms

NAFLD is often asymptomatic, but some people experience fatigue/ tiredness, right upper abdominal discomfort, and unexplained weight loss. Advanced disease may cause jaundice, swelling, confusion, and easy bruising, redness in the palm called liver palm (palmar erythema), and red spots on the upper part of the chest called spider naevi.
NAFLD/MASLD is frequently silent; thus, screening and routine checkups are essential for early detection in those who are at risk.
📋Diagnosis of NAFLD

NAFLD/MASLD is typically diagnosed incidentally during routine medical tests when liver function tests show abnormalities or imaging studies detect fat in the liver. The diagnosis involves clinical evaluation, blood tests, imaging studies, and sometimes a liver biopsy.
| Diagnostic Tool | Purpose | Comments |
|---|---|---|
| Blood Tests | Liver enzymes, glucose, lipids | First-line screen |
| Imaging | Fat and fibrosis detection | Ultrasound, FibroScan, MRI |
| Scoring Systems | Estimate fibrosis | FIB-4, APRI, NFS |
| Biopsy | Confirm NASH | Used selectively |
| Risk Screening | Identify at-risk | Metabolic syndrome, obesity |

Scoring System
📊 FIB-4 Index Calculator
Enter the values below to calculate the FIB-4 index for liver fibrosis.
Note: For interpretation, check this page link >>https://livertransplanthelp.com/fib-4-index-calculator/
FIB-4 (Fibrosis-4 Index):
A quick, non-invasive calculation using your age, liver enzymes (AST & ALT), and platelet count to estimate if your liver might have fibrosis (scarring). Helps determine if additional tests are necessary.
A FIB-4 score of ≥ 1.3 [ FIB-4 thresholds 1.3 valid for age ≤35 years or >65 years: Higher FIB-4 cut-off is 2.0 for older patients] may indicate the presence of fibrosis and warrants further evaluation with a secondary fibrosis assessment method (VCTE, MRE). Tests of specific collagen-related blood constituents (e.g. enhanced liver fibrosis [ELF]) may serve as an alternative to imaging to identify advanced liver fibrosis
Note : Non-invasively obtained blood-based biomarkers (such as FIB-4 and ELF) and measurements of liver stiffness (vibration-controlled transient elastography [VCTE] or magnetic resonance elastography [MRE])are suitable for reliably detecting advanced fibrosis.
NFS (NAFLD Fibrosis Score):
A broader liver health check that combines age, BMI, platelets, albumin, AST/ALT ratio, and whether you have diabetes or prediabetes, to assess the risk of advanced fibrosis in fatty liver disease.
APRI (AST to Platelet Ratio Index):
A simple score using just AST levels and platelet count to give a quick idea of whether there might be liver scarring, especially useful when imaging or biopsy isn’t available.
📋 Fibroscan Interpretation
FibroScan (VCTE/Vibration-Controlled Transient Elastography) is a specialised ultrasound procedure that evaluates liver stiffness and fat accumulation using shear wave technology.
People with the following conditions are advised to get a Fibroscan:
- Suspected NAFLD/MASLD or NASH/MASH
- Elevated liver enzymes (ALT, AST)
- Chronic hepatitis B or C
- Obesity or type 2 diabetes
- History of alcohol abuse
- Tracking the course of liver disease or recovery after treatment
| Component | Range | Interpretation |
|---|---|---|
| Liver Stiffness (kPa) | < 7 | No significant fibrosis |
| 7–14 | Significant fibrosis (F2–F3) | |
| > 14 | Cirrhosis (F4) | |
| CAP Score (dB/m) | < 238 | No steatosis |
| 238–260 | Mild steatosis | |
| 260–290 | Moderate steatosis | |
| > 290 | Severe steatosis |
🩻 FibroScan = Liver ultrasound 2.0
- Stiffness (kPa) tells us how scarred your liver is (F0–F4 scale). ≥8.0 kPa is taken as significant, needs Hepatology referral. Diagnostic work-up and management plan for liver-related outcomes. Intensified management of comorbidities (in a multidisciplinary team)
- Controlled Attenuation Parameter/ CAP Score (dB/m) shows how fatty your liver is (none → severe).
- Non-invasive, quick, painless — often used in NAFLD, NASH, hepatitis, or alcohol-related liver disease.
🧠 What Are the NAFLD/MASLD Treatment Options Available?
There’s no magic pill yet — but treatment is all about hitting the roots: weight, sugar, fat, and inflammation.

| Treatment Modality | Description |
|---|---|
| 🥦 Lifestyle Changes | Considered for patients with severe obesity (BMI >35) and progressive NAFLD. It can significantly reduce liver fat and inflammation. |
| 💊 Medications | - Vitamin E: For non-diabetics with NASH (antioxidant). - Pioglitazone: Improves insulin sensitivity (diabetics). - GLP-1 receptor agonists: e.g., semaglutide, reduce liver fat and support weight loss. |
| 🏥 Bariatric Surgery | Considered for patients with severe obesity (BMI >35) and progressive NAFLD. It can significantly reduce liver fat and inflammation. |
| 🩺 Liver Transplant | Reserved for advanced cirrhosis or liver failure due to NASH. Not a routine NAFLD solution. |
What are the Lifestyle Changes recommended for NAFLD/MASLD?
CDC recommends :
- Aim to lose 1 to 2 pounds (0.5 to 1 kilogram) a week over the long term, which can reduce liver and other visceral fat, plus reduce liver inflammation.
- 5% to 10% weight loss of your starting weight in 6 months.
- Sudden loss in weight, especially with calorie restriction, can lead to fatty liver /NASH,/Cirrhosis.
According to EASL guidelines, weight loss through dietary and behavioural therapy is highly recommended for individuals with FLD who are overweight or obese. The goal is to maintain a reduction of ≥5% to reduce liver fat and 7–10% to ameliorate liver inflammation. Nearly complete non-alcoholic steatohepatitis resolution and at least one stage improvement in fibrosis can be achieved with weight reductions of ⩾10%.
The term "lean NASH" describes non-alcoholic steatohepatitis (NASH) that affects people who are not overweight or obese. This stands in contrast to the more widely recognised link between NASH and metabolic syndrome and obesity.

🍎 Food is Medicine: Eat Smart, Heal Better. Lifestyle changes begin with your plate.
👉 Download the Free Liver Food Guide — A doctor-approved cheat sheet for liver-friendly meals that reduce fat and inflammation. Fill up the subscription form for a free download.
🥗 Sample Diet for Liver Health: What Should a NAFLD Plate Look Like?
Smart substitutions are the key to a liver-friendly diet, not starvation. High-fibre vegetables, whole grains, lean proteins (such as tofu, salmon, and lentils), unsweetened coffee or green tea, and healthy fats like walnuts and olive oil should all be prioritised. Reduce red meat, processed meals, and refined sugar.
☕ Is Coffee Good for NAFLD/MASLD?
Yes — moderately!
Several studies suggest that drinking coffee (especially black coffee) is associated with:
- ✅ Reduced liver fat accumulation
- ✅ Lower risk of liver fibrosis
- ✅ Improved liver enzyme levels
- ✅ Slower progression of NAFLD to NASH or cirrhosis
🔍 Why Does Coffee Help?
Coffee contains:
- Caffeine helps reduce fat buildup
- Chlorogenic acid – an antioxidant and anti-inflammatory
- Diterpenes (like cafestol) may protect against fibrosis
These compounds help reduce oxidative stress and improve insulin sensitivity, both key in managing NAFLD.
☕ How Much Coffee is Good?
- 2–3 cups/day of plain, unsweetened black coffee shows benefit.
- Avoid excessive sugar, cream, and syrups — they reverse the benefits.
- Filtered coffee is preferred over unfiltered (e.g. French press), as unfiltered coffee has higher diterpenes, which may raise LDL.
⚠️ Who Should Be Careful?
- People with acid reflux, insomnia, or uncontrolled hypertension
- Avoid overconsumption (4+ cups daily) unless tolerated
- Always consult your doctor if you’re on medications or have other conditions
💊 What is Resmetirom?
✅ Resmetirom (Brand: Rezdiffra)
FDA-approved first-in-class treatment for:
👉 MASH (Metabolic dysfunction–Associated Steatohepatitis)
👉 With moderate to advanced fibrosis (F2–F3)
🚀 Why It’s a Game-Changer:
| Evidence From Trials | Highlights |
|---|---|
| 🧪 MAESTRO-NASH & MAESTRO-NAFLD-1 | - Reversal of steatohepatitis - Fibrosis improvement without worsening other parameters |
| 🧠 How It Works | Thyroid hormone receptor-β agonist → regulates fat metabolism in the liver. |
🧬 Who Is Eligible for Resmetirom?
Think cardiometabolic risk + liver fibrosis (but not cirrhosis).
| Criterion | Details |
|---|---|
| ✅ Confirmed F2–F3 Fibrosis | Via non-invasive tests: -FibroScan (VCTE/Vibration-Controlled Transient Elastography),-MRE, MRI-PDFF (Magnetic Resonance Imaging Proton Density Fat Fraction). |
| ✅ Evidence of Steatosis | CAP Score /Controlled Attenuation Parameter |
| ✅ Cardiometabolic Risk Factors | Obese, Diabetic, or Metabolic syndrome patients, Dyslipidemia |
| ❌ Exclusions | Cirrhosis, untreated thyroid disease, and active alcohol use. |
📈 Monitoring Response to Resmetirom
| Method | Purpose |
|---|---|
| 🧪 Liver Function Tests | Regular ALT/AST monitoring. |
| 📊 Non-Invasive Imaging (NILDA) | MRI-PDFF, FibroScan for fat & fibrosis regression. |
| 🧬 Biomarkers | ALT drop, improved liver stiffness (kPa), and lower triglycerides. |
🌿 Supplements & Herbal Products/so-called liver Detox: What to Know
Natural doesn't always mean safe. Curcumin (turmeric extract), silymarin (milk thistle), omega-3, and green tea extract are commonly promoted as “liver detox” remedies — a popular but misleading term. While some of these compounds may have antioxidant or anti-inflammatory effects, their safety and efficacy depend heavily on the dose, formulation, and individual liver status. Several herbal or ayurvedic products can cause liver injury. During the COVID-19 wave, "we saw many patients who needed a transplant because of liver injury caused by giloy" (Tinospora cordifolia) — often taken without supervision. Self-prescribing supplements is risky. Always consult a healthcare provider before adding any herb or product to your wellness routine.
🩹 Monitoring and Follow-Up Plan
NAFLD is not a one-time diagnosis.
- Repeat LFTs should be performed every three to six months, followed by an ultrasound or FibroScan once a year, and routine measurements of blood glucose, HbA1c, waist circumference, and BMI.
- High-risk individuals should have their fibrosis scores (FIB-4, NFS, etc.) repeated in order to evaluate the course of their disease and determine whether they require referral to a specialist.
What Causes Fatty Liver Disease in Children?
Obesity and insulin resistance are the main causes of fatty liver disease in children, which is medically referred to as non-alcoholic fatty liver disease (NAFLD) or metabolic dysfunction-associated steatotic liver disease (MASLD). A sedentary lifestyle, poor eating habits, genetic susceptibility, metabolic syndrome, hypertension, and high cholesterol/triglyceride levels are all contributing factors. Even while juvenile NAFLD is frequently quiet in its early stages, if left untreated, it can eventually cause fibrosis, inflammation (MASH), and even cirrhosis.
🧒 Management in children revolves around structured lifestyle intervention, and one of the most effective and easy-to-remember tools is the 5-2-1-0 rule, endorsed by the Indian Academy of Paediatrics (IAP):
- 5 servings of fruits and vegetables per day
- 2 hours or less of recreational screen time
- 1 hour of physical activity every day
- 0 sugar-sweetened beverages
This IAP-recommended framework empowers families to adopt daily habits that promote liver health, reduce obesity, and reverse early liver changes. Timely lifestyle changes, when supported by family and schools, can significantly reduce the risk of long-term liver damage.
🤰 NAFLD and Pregnancy: A Growing Concern
Gestational diabetes, preeclampsia, premature birth, and even cesarean sections are among the issues that women with NAFLD are more likely to experience. For women who are pregnant or considering a pregnancy, lifestyle management and screening are essential. Weight, blood pressure, and blood sugar control can all contribute to safer outcomes for both the mother and the fetus.
🧠 Psychosocial Impact of NAFLD
Living with NAFLD/MASLD has an impact on mental and emotional well-being in addition to physical health. Chronic weariness, mental fog, and even embarrassment or stigma are common complaints from patients, particularly when their physical appearance doesn't correspond with the "look" of liver illness. Emotional support, knowledge, and empathy are all crucial components of comprehensive care.
✅ Take-Home Message: What You Need to Remember About NAFLD/MASLD

🔹 NAFLD (Non-Alcoholic Fatty Liver Disease) is now reclassified as Steatotic Liver Disease (SLD), with subtypes like MASLD, MetALD, and MASH.
🔹 MASLD = Fat in liver + ≥1 cardiometabolic risk factor, regardless of alcohol intake level.
🔹 Cardiometabolic Risk Factors Include:
- BMI ≥ 25 kg/m²
- Waist Circumference > 90 cm (men), > 80 cm (women)
- Fasting glucose > 100 mg/dL or HbA1c > 5.7%
- BP ≥ 130/80 mmHg
- Triglycerides > 150 mg/dL
- HDL < 40 mg/dL (men) / < 50 mg/dL (women)
🔹 MASH (Metabolic dysfunction-associated Steatohepatitis) replaces NASH — it means fat + inflammation + liver cell injury, with metabolic roots.
🔹 MetALD is a combination of metabolic dysfunction and alcohol-related fatty liver, not either/or.
🔹 MASLD can coexist with:
- Autoimmune hepatitis
- Viral hepatitis (HBV/HCV)
- Drug-induced liver injury
- Genetic/metabolic liver diseases
🔹 Diagnosis is often incidental, through abnormal liver enzymes or fatty changes seen on ultrasound.
🔹 Scoring Systems like FIB-4, NFS, APRI, and FibroScan help assess fibrosis risk non-invasively.
🔹 FibroScan Key Values:
- Liver stiffness > 7 kPa = significant fibrosis
- CAP score > 290 dB/m = severe steatosis
🔹 Lifestyle Is the First-Line Treatment:
- Aim for 5–10% weight loss over 6 months
- Avoid crash dieting — it may worsen liver injury
- Adopt a liver-friendly diet, regular activity, and stress management
🔹 Coffee (2–3 cups/day) is protective — reduces liver fat, fibrosis, and inflammation (without sugar/cream)
🔹 Resmetirom (Rezdiffra) is the first approved drug for MASH with moderate fibrosis, not for cirrhosis
🔹Pediatric fatty liver disease (NAFLD/MASLD) is rising, largely driven by obesity and insulin resistance.
Early stages are often silent, but progression to liver damage is real and preventable.
The Indian Academy of Paediatrics (IAP) recommends the 5-2-1-0 rule as a powerful lifestyle guide:
- 5 servings of fruits & vegetables daily
- 2 hours or less of screen time
- 1 hour of physical activity
- 0 sugary drinks
Small daily changes at home and school can reverse early fatty liver, improve metabolic health, and protect the future of our children.
👩⚕️🧠Final Wisdom

New terms like MASLD and MASH help remove stigma and refocus care on real causes
MASLD is not “just fatty liver — it’s part of a broader metabolic disorder.
Early lifestyle changes and risk detection can REVERSE damage and save lives
Frequently Asked Questions
Q1: What is MASLD, and how is it different from MetALD or ALD?
A1: MASLD (Metabolic dysfunction-associated steatotic liver disease) is liver fat accumulation due to metabolic dysfunction. MetALD includes both metabolic risk and moderate alcohol intake, while ALD is caused mainly by excessive alcohol use.
Q2: Can a person have MASLD along with another liver disease?
A2: Yes. The new SLD terminology allows dual diagnoses, such as MASLD with autoimmune hepatitis or viral hepatitis. These require separate evaluation and treatment.
Q3: How is NAFLD diagnosed?
A3: NAFLD is often detected incidentally through abnormal liver tests or imaging. Diagnosis includes blood tests, imaging (like FibroScan or MRI-PDFF), non-invasive scoring tools, and sometimes liver biopsy.
Q4: What is FibroScan, and how are the results interpreted?
A4: FibroScan is a non-invasive test that measures liver stiffness and fat. A stiffness below 7 kPa is normal; above 7 suggests fibrosis, and above 14 kPa indicates cirrhosis. CAP scores help determine fat levels.
Q5: What are the main treatment options for NAFLD?
A5: Lifestyle changes are key. Vitamin E, pioglitazone, or GLP-1 agonists may help. Bariatric surgery or liver transplant is considered in advanced cases. Resmetirom is a new FDA-approved drug for MASH with fibrosis.
Q6: What is Resmetirom, and who is eligible for it?
A6: Resmetirom is approved for MASH patients with F2–F3 fibrosis. It's prescribed based on non-invasive tests like FibroScan or MRI elastography, especially in patients with metabolic risk factors and no significant alcohol use.
Q7: How is treatment response monitored in MASH patients?
A7: Response to Resmetirom is monitored using liver function tests, ALT levels, and imaging tools like FibroScan or MRI-PDFF. Improvement in liver stiffness and enzyme levels indicates a good response.
Q8: Is drinking coffee good for NAFLD?
A8: Yes, moderate coffee consumption (2–3 cups a day) has been associated with reduced liver fat, lower liver enzyme levels, and slower disease progression in people with NAFLD.
Coffee contains antioxidants and anti-inflammatory compounds that may help protect the liver. However, skip the sugar and cream — black or minimally sweetened coffee is best.
🎉 First Consultation with Dr. Tanuja Mallik is FREE!
Get expert advice on liver transplant, recovery, and care — at no cost.
Book your free WhatsApp consultation now:
✅ After booking, please send a WhatsApp message to confirm your slot.
📞 Only first call is free. Follow-ups: ₹499 per session.
Thanks a lot for sharing the article.
Welcome Sonali 🙂