🔻 Base: Paracetamol Basics
Paracetamol (Acetaminophen) is a commonly used pain and fever reliever.
It’s safe when taken as prescribed, available over the counter.
Works by blocking the COX-2 enzyme to reduce pain signals and lower temperature.
⚠️ Layer 2: Overdose Risk – Who’s Vulnerable?
Elderly, children, chronic alcohol users, and those with liver disease are at higher risk.
Multiple products (e.g. cold & flu meds) may contain hidden paracetamol.
Taking slightly more than the safe dose over several days can cause silent liver damage.
🎯 Layer 3: Know the Safety Margin
Maximum adult dose: 4,000 mg/day (8 tablets of 500 mg) — never exceed this
Therapeutic window is narrow: small excess = big risk
Keep at least a 4–6 hour gap between doses
Always check labels for combined meds (avoid doubling unknowingly)
🧠 Top: Smart Knowledge = Smart Use
Don’t mix with alcohol 🍷
Use weight-based dosing for children
Be cautious in fasting, underweight, or malnourished states
In case of suspected overdose: Seek help within 8 hours — NAC can save the liver!
Remember: OTC doesn’t mean risk-free
Ah, paracetamol—the overachiever of medicine cabinets and handbags across the globe. Got a headache? Pop one. Period cramps? Two more, just in case. Fever? You already know the drill. It’s the go-to remedy for everything from mild discomfort to full-blown “I can’t adult today” emergencies. Cheap, cheerful, and available over the counter like candy. What could go wrong?
Well… enter the dark horse: paracetamol overdose.
Yup, that seemingly innocent white pill can turn into a silent liver assassin if not handled with care. Most people don’t realise that the same drug we trust for quick relief has a very narrow safety margin. Just a few extra doses over the recommended limit—and bam—you’re in risky territory. We’re talking serious liver damage, and in extreme cases, even liver failure.
In fact, according to the American Association of Poison Control Centres, over 66,000 cases of paracetamol overdose were reported in the U.S. in 2022 alone, leading to nearly 200 deaths. And globally, it’s one of the top causes of sudden liver failure, even overtaking viral hepatitis in countries like the U.S. and the U.K.
But before you freak out and swear off painkillers forever, breathe. This blog isn’t here to scare you—it’s here to arm you with smart knowledge. We’ll break down exactly how paracetamol works, what qualifies as a paracetamol overdose, what warning signs to watch for, and how to stay safely within the “relief” zone without crossing into “uh-oh” land.
Ready to bust some myths, dodge the dangers, and get the facts without the jargon? Let’s roll into this KYM (Know Your Medicine) special with curiosity, a sprinkle of humour, and a healthy respect for your liver.
What’s the Deal with Paracetamol?
(How Does It Work?)

Paracetamol—also known as acetaminophen—is one of the most widely used painkillers and fever reducers around. Found in almost every household, it’s often the first remedy we reach for when a headache, muscle ache, or fever strikes.
But how does it work?
Mechanism of action: Paracetamol works by blocking the production of prostaglandins( blocks an enzyme called COX-2, which is in charge of producing prostaglandins), chemicals in the brain that signal pain and elevate body temperature. Unlike drugs like ibuprofen or aspirin, it doesn’t reduce inflammation, so it’s not the best choice for swelling or injuries that involve redness or heat. But for non-inflammatory issues like tension headaches or mild fevers, it does the job—and it does it well.
But here’s where caution is critical: its safety profile has limits.
People often assume that since it’s available over the counter, paracetamol is completely harmless. Unfortunately, this assumption is what leads to accidental paracetamol overdose, a major cause of liver damage around the world. Even slightly exceeding the recommended dose over several days can quietly overwhelm your liver before symptoms even appear.
So yes—it’s effective.
But if misused, it can be dangerous.
What Can Go Wrong?
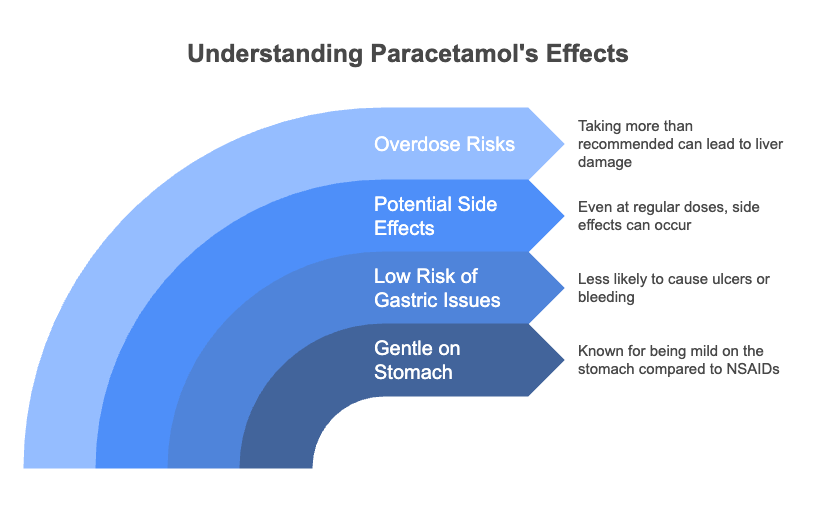
Paracetamol is often praised for being gentle on the stomach, especially when compared to heavy hitters like NSAIDs (aspirin or ibuprofen). It’s the darling of over-the-counter meds, loved for its low risk of causing gastric ulcers or bleeding. But here’s the twist: just because it’s well-tolerated doesn’t mean it’s risk-free.
Even at regular doses, side effects can pop up, and if you start taking more than you should, you’re heading into dangerous territory—specifically, a paracetamol overdose, which can lead to liver damage and even liver failure.
Possible Side Effects
Most people won’t experience side effects when they stick to the correct dose, but here are a few to watch for:
- Nausea & Vomiting – Your body’s not vibing with the extra dose.
- Fatigue or Weakness – That sluggish, “I need a nap immediately” feeling.
- Abdominal Pain – Especially in the upper right side (your liver might be waving a red flag).
- Headaches – Yep, the irony is real.
- Rashes or Itchy Skin – Signs of an allergic reaction or sensitivity.
Mild, yes. But let these serve as a gentle nudge that paracetamol isn’t just a candy-like fix. Now, what happens if someone crosses the line from “safe use” to “oops, I took too much”?
The Tipping Point: Paracetamol Overdose

A paracetamol overdose doesn’t always announce itself with dramatic symptoms—at least not right away. That’s what makes it sneaky and dangerous. People often take slightly too much over several days, especially when using multiple cold or flu medications that all contain paracetamol (hello, unintentional stacking).
Recommended Dosage Guidelines
To avoid slipping into dangerous territory, here’s what the experts say:
🔹 Adults
- Maximum dose per intake: 500 mg to 1000 mg
- Maximum daily dose: 4000 mg (4 grams) within 24 hours
- Minimum gap between doses: 4 to 6 hours
🔹 Children (always based on weight & age)
- 10–15 mg per kilogram of body weight per dose
- Repeat every 4–6 hours, but no more than 5 doses in 24 hours
- Never guess—use a dosing chart or paediatric advice if unsure
⚠️ Paracetamol Drug Interactions:
What You Should Know

Paracetamol is one of the safest painkillers when used appropriately. But when taken alongside certain medications or substances, the risk of side effects or even toxicity increases, especially with repeated and higher cumulative doses. Here are the key interactions to be aware of:
| Drug/Group | Interaction Type | Mechanism | Clinical Recommendation |
|---|---|---|---|
| Alcohol (Ethanol) | Synergistic hepatotoxicity | Chronic alcohol use induces CYP2E1, increasing toxic NAPQI metabolite formation; glutathione depletion increases liver injury risk. | Avoid alcohol completely if taking regular/high-dose paracetamol. Essential in liver disease or alcohol use disorder. |
| Warfarin | Increased anticoagulant effect | Possible interference with vitamin K metabolism; chronic paracetamol use raises INR. | Limit to short-term use. Monitor INR if used >3 days. Adjust warfarin dose as needed. |
| Phenytoin, Carbamazepine | Reduced efficacy & increased hepatotoxicity | Induce hepatic enzymes (e.g., CYP450), increasing toxic metabolite production and reducing analgesic effect. | Avoid frequent/repeated dosing. Monitor LFTs regularly if concurrent use is needed. |
| Isoniazid, Rifampin | Additive hepatotoxicity | Compete for hepatic metabolism; increased NAPQI production + intrinsic hepatotoxicity. | Use with caution. Regular liver function monitoring advised. Require physician supervision. |
| Pregnancy | Generally safe | Crosses placenta; no clear teratogenicity at therapeutic doses. | Use only when needed. Avoid prolonged/high-dose use. |
| Lactation | Safe | Minimal amounts secreted in breast milk; no adverse infant outcomes reported. | Considered compatible. Monitor infant if used repeatedly. |
| G6PD Deficiency | Rare risk of hemolysis | Mild oxidative stress possible but not common. | Use with caution. Avoid excessive dosing. Monitor for hemolysis signs. |
| Liver Disease | Increased toxicity risk | Impaired metabolism, reduced clearance, low glutathione levels. | Max 2g/day, spaced doses. Monitor LFTs. Avoid self-medication. |
| Chronic Alcohol Use | High hepatotoxicity risk | CYP2E1 induction + depleted antioxidants = amplified NAPQI toxicity. | Strongly contraindicated unless under medical supervision. Use lowest possible dose. |
🧠
Paracetamol is safe and effective, but not without exceptions. Avoid self-medicating when multiple drugs or health conditions are involved.
🚨Paracetamol Overdose Risks
Paracetamol is often seen as a mild-mannered superhero in the medicine cabinet. But even heroes have their limits. The line between safe use and overdose is thinner than most people realise—and crossing it could lead to serious consequences.
🧪 How Much is Too Much?
| Parameter | Details |
|---|---|
| Toxic Dose (Single Ingestion) | >150 mg/kg in adults or children (≈7.5 g in adults) |
| Toxic Serum Level (per Rumack-Matthew Nomogram) | Serum paracetamol concentration >150 μg/mL at 4 hours post-ingestion |
| Time Frame Considered for Overdose | Single ingestion within ≤8 hours |
| Threshold for Treatment with NAC (N-acetylcysteine) | If serum paracetamol crosses or is above the “treatment line” on Rumack-Matthew Nomogram at 4–24 hours |
| Chronic or Staggered Overdose (e.g., therapeutic misadventure) | Lower thresholds apply; NAC may be started even at lower cumulative doses if risk factors (e.g., malnutrition, chronic alcohol use, liver disease) are present |
For adults, the safe dose is:
- 500 mg to 1000 mg per dose,
- Every 4 to 6 hours,
- With a maximum of 4,000 mg (4 grams) in 24 hours.
But here’s the catch: just two extra tablets over the max dose can shift things from “safe” to “risky.”
An acute overdose is typically anything over 7.5 grams (7,500 mg) in one go—that’s just 15 standard 500 mg tablets. It sounds like a lot, but during feverish days or painful nights, it can happen without much thought.
For children, doses must always be based on weight, typically 10–15 mg/kg per dose, every 4–6 hours, not exceeding 60 mg/kg in 24 hours. Overdose in kids can be more dangerous, as symptoms might appear late but progress rapidly.
💥 What Happens in a Paracetamol Overdose?

🧬 Pathophysiology
Glutathione Role: NAPQI is detoxified by glutathione; in overdose situations, glutathione stores are depleted, leading to hepatocellular damage.
Metabolism: At therapeutic doses, paracetamol is primarily metabolised in the liver through glucuronidation and sulfation.
Toxic Metabolite: A small fraction is metabolised by cytochrome P450 enzymes to form N-acetyl-p-benzoquinone imine (NAPQI), a toxic compound.
😰 Signs and Symptoms of Overdose
The scary part? Symptoms often don’t show up right away. People may feel “okay” for the first 24 hours, but that’s when silent liver damage is already brewing. Here’s how the timeline usually plays out:
🩺 Clinical Stages of Toxicity
Stage I (0–24 hours): Nausea, vomiting, malaise, and diaphoresis; patients may be asymptomatic.
Stage II (24–72 hours): Right upper quadrant abdominal pain, elevated liver enzymes, and possible renal dysfunction.
Stage III (72–96 hours): Peak hepatotoxicity with jaundice, coagulopathy, hypoglycemia, encephalopathy, and possible death.
Stage IV (4 days–2 weeks): Recovery phase for survivors; liver function may return to normal.
🧪 Diagnosis
- Serum Acetaminophen Levels: Measured 4 hours post-ingestion; levels plotted on the Rumack-Matthew nomogram to assess hepatotoxicity risk.
- Laboratory Tests: Liver function tests (LFTs), coagulation profile (PT/INR), renal function tests, and electrolytes.
- Imaging: Not routinely required but may be used to assess liver size and rule out other causes of symptoms.
💊 Treatment
Liver Transplantation: Considered in cases of fulminant hepatic failure unresponsive to medical therapy.
N-Acetylcysteine (NAC): Antidote that replenishes glutathione stores and enhances non-toxic metabolism of acetaminophen. Most effective when administered within 8 hours of overdose.
Activated Charcoal: May be administered within 1–2 hours of ingestion to reduce absorption.
Supportive Care: Monitoring and management of complications such as hypoglycemia, coagulopathy, and encephalopathy.
👥 Prevention Strategies
- Public Education: Informing patients about the risks of overdose and the presence of acetaminophen in combination products.
- Healthcare Provider Role: Counselling patients on appropriate dosing and monitoring for signs of toxicity.
- Regulatory Measures: Implementing labelling changes and limiting the amount of acetaminophen per dosage unit in over-the-counter products.
✅ Key Takeaway
- Paracetamol is powerful, but precision matters.
- Never exceed the daily limit.
- Always check if other medications (like cold or flu combos) contain paracetamol to avoid accidental doubling up.
- And if in doubt, t—ask your doctor.
Frequently Asked Questions
Q1: What is the safe dose of paracetamol for adults?
A1: The usual adult dose is 500–1000 mg every 4–6 hours, not exceeding 4000 mg in 24 hours.
Q2: How much paracetamol is considered an overdose?
A2: Taking more than 4000 mg in 24 hours can lead to liver damage or overdose.
Q3: What are the signs of a paracetamol overdose?
A3: Early signs may include nausea, vomiting, and abdominal pain. Severe cases can cause liver failure, confusion, or even coma.
Q4: Can I drink alcohol while taking paracetamol?
A4: It’s best to avoid alcohol, as both alcohol and paracetamol are processed by the liver and can increase the risk of liver toxicity.
Q5: What should I do in case of overdose?
A5: Seek emergency medical help immediately. Activated charcoal, N-acetylcysteine (NAC) may be given as an antidote if treated early.
Q6: Is paracetamol addictive?
A6: No, paracetamol is not addictive, but chronic overuse can create a harmful habit and serious health risks.
Q7: Can I give paracetamol to children?
A7: Yes, but only in age-appropriate doses. Always use the pediatric formulation and consult a doctor.
🧭 Wrapping It Up: Respect the Pill, Protect Your Liver
Paracetamol is a modern-day marvel—safe, effective, and easy to access. But like all powerful tools, it comes with responsibility. When taken correctly, it’s your ally against everyday aches and fevers. But misuse, whether intentional or accidental, can turn it into a silent threat to your liver.
The key? Know your doses. Know your risks. And when in doubt, ask.
Always read labels carefully, check for hidden paracetamol in combination meds, and avoid mixing it with alcohol or interacting drugs.
This isn’t about creating fear—it’s about creating awareness. The more you understand your medicine, the more empowered you become in protecting your health or the health of your loved ones.
💬 “Medicine is not just science, it’s wisdom in practice.”
— And knowing when not to take a pill is just as important as knowing when to take one.
👩⚕️ This article is part of the KYM (Know Your Medicine) series—a compassionate guide from a liver transplant doctor to help patients and caregivers make safe, smart decisions, one medicine at a time.
🌐 Connect with Me — Anywhere, Anytime
Looking for Web Stories, wellness blogs, trusted liver health resources, or just want to ask me something directly?
🔗 Tap into my full digital world — all in one place:
👉 Dr. Tanuja’s Wellness LinkTree
Inside, you’ll find:
- 📲 WhatsApp — message me directly
- 📘 Facebook — follow updates & videos
- 📸 Instagram — wellness reels & behind-the-scenes
- 🎥 YouTube — expert insights coming soon
- 🖼️ Pinterest — healing visuals & wellness pins
- 🧵 Twitter — thoughts, threads & updates
- 🎙️ Spotify — Liver Transplant Insight podcast
- 🛍️ Instamojo Shop — digital products, guides & more
- 🛒 Website Shop — handpicked recovery tools
- 🌿 Web Stories — snackable expert health tips
- 💼 LinkedIn — professional updates and connections
About the Author Dr. Tanuja Mallik is a liver transplant anaesthetist and critical care specialist with years of experience in managing complex transplant cases.
Disclaimer This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider for personalised guidance.
“How many people are popping paracetamol without checking their liver? 🫣
Ever wondered if your lifestyle is silently hurting your liver?
Drop a 🧠 if you want me to decode it — or just type YES.”