Pre-liver transplant counselling doesn’t start with a signature. It starts with a conversation.
In real-world clinical practice, counselling begins the very first time a patient walks into the liver transplant clinic and meets the eligibility criteria. From that point, it becomes a continuous, evolving process involving not just the patient but the family, the potential donor, and the entire multidisciplinary team.
Once the patient agrees to undergo a transplant, a parallel process unfolds:
- Medical and psychological evaluations begin
- The patient and family are counselled about both LDLT and DDLT options
- Expectations are set, fears are addressed, and decisions are made step by step
This is not a one-time briefing. It often involves multiple counselling sessions across days or even weeks, including a final, detailed counselling on the day of the transplant, where informed consents are reconfirmed and every question is answered once again.
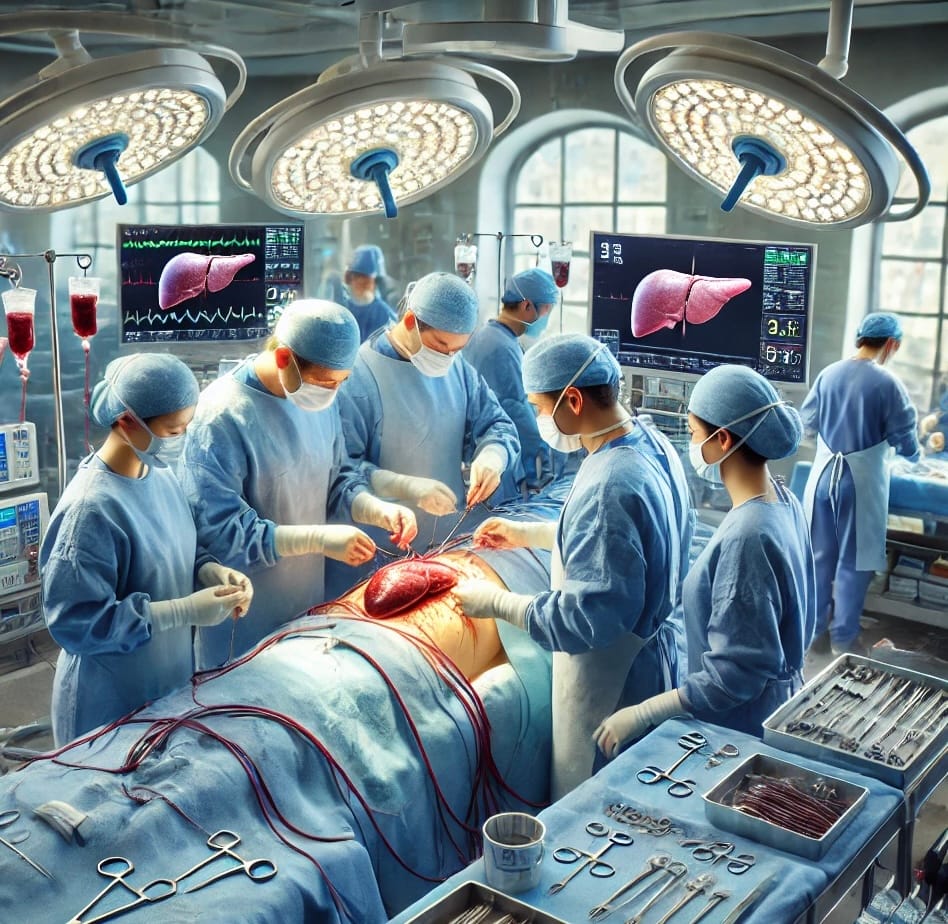
For patients with acute liver failure or end-stage liver disease, liver transplantation is often the only hope and the right pre-transplant preparation can be the difference between just surviving and truly thriving after surgery. In particular, Living Donor Liver Transplant (LDLT) has emerged as a preferred option due to reduced wait times and better survival rates.
But here’s the truth few talk about: Surgery alone doesn’t guarantee success.
Success begins before you ever reach the OT — it begins with something often overlooked: Pre-liver transplant counselling.
What is LDLT, or living donor liver transplant?
A healthy liver part is surgically removed from a living donor and given to the recipient in LDLT. Both the recipient’s and donor’s livers can regain their full size in a matter of months, thanks to the liver’s special capacity for regeneration. In areas with a shortage of deceased donor organs, this process is especially helpful.
We value every patient and every donor. In the case of a living donor liver transplant, donor safety is paramount.
- If the first donor evaluation reveals any concerns, we immediately explore alternate options
- Families are told in advance that: donation will happen only if the donor is deemed completely fit
- Every risk, benefit, and doubt is thoroughly addressed for both the donor and the recipient
🔁 Dual Listing: DDLT and LDLT
In many cases, patients may be listed for both deceased donor liver transplant (DDLT) and living donor liver transplant (LDLT).
- If a cadaver organ becomes available in time, they are taken up for DDLT
- If not, and a suitable family donor is available, the team may proceed with LDLT
- This flexibility in planning helps reduce waiting time and optimise outcomes
What Makes Pre-Liver Transplant Counselling Crucial?

🌱 Informed Decision-Making: Both the patient and the donor are educated and prepared for the procedure and its aftermath through the extensive process of pretransplant counselling. It guarantees well-informed decision-making, lowers anxiety, and establishes reasonable expectations.
🧠 Mental & Emotional Preparedness: The recipient and donor must be fully cognizant of the procedure’s dangers, advantages, and available options. Counselling helps handle the substantial emotional and mental effects of surgery.
🩺 Risk Identification & Mitigation: A comprehensive medical evaluation is part of counselling to make sure both individuals are mentally and physically prepared for the process.
📊 Expectation Management: Following a transplant, both donors and recipients must be aware of the long-term health effects and lifestyle adjustments.
🔐 Ethical Safeguards: Protects against coercion, misinformation, or guilt-driven decisions.
Important Aspects of Pre-Liver Transplant Counselling

- For the Recipient, evaluate the severity of liver disease and ascertain the transplant’s urgency.
- Assess general health, including kidney, lung, and cardiac function.
- Talk about possible side effects, including infection, rejection, or biliary problems.
- Make sure the donor is in good health and free of any underlying disorders that could raise the risk of surgery.
- Perform imaging studies to evaluate the volume and anatomy of the liver.
- Examine the dangers of surgery, such as the possibility of bleeding, infection, and uncommon side effects such as liver failure.
2. Psychological and Emotional Support
- For the Recipient: Address fears and anxieties about the surgery and recovery process. Provide coping strategies for the emotional toll of chronic illness and transplantation.
- For the Donor: Ensure the donor is volunteering willingly without coercion. Discuss the emotional impact of donating an organ and provide resources for mental health support.
3. Legal and Ethical Considerations
- Both parties must understand the legal aspects of organ donation, including consent forms and the donor’s right to withdraw at any time.
- Ethical considerations, such as ensuring the donor’s autonomy and the recipient’s best interest, are also discussed.
4. Financial Counselling
- Liver transplantation can be expensive, and both the donor and recipient need to understand the costs involved.
- Discuss insurance coverage, out-of-pocket expenses, and potential financial assistance programs.
5. Post-Transplant Care and Lifestyle Changes
- For the Recipient: Educate about lifelong immunosuppressive medications and their side effects. Discuss dietary changes, exercise, and regular follow-ups.
- For the Donor: Provide guidelines for recovery, including activity restrictions and follow-up care. Discuss the timeline for liver regeneration and long-term health monitoring.
🧾 Knowing the Liver Transplant Waitlist for Cadaver Donation: Essential Information for Patients and Their Families
A cadaver (dead donor) liver transplant waitlist is used when a patient needs a liver transplant but a living donor is either unavailable or unsuitable. The regional organ transplant authority is responsible for maintaining this list, which is closely coordinated with your liver transplant team.
The Liver Transplant Waitlist: What Is It?
The National Organ and Tissue Transplant Organization (NOTTO) oversees the distribution of cadaver organs in India, working with the State-level SOTTO and regional ROTTO networks. Your transplant hospital adds your name to this consolidated waiting list as soon as you are given the all-clear for a liver transplant.
🩺 How Is Priority Determined?
The ranking is not just first-come, first-served. It depends on several medical and logistical factors:
| Criteria | What It Means |
|---|---|
| MELD Score | A score (6 to 40) based on lab values — higher = more urgent |
| Blood Group Matching | The donor’s liver must match your blood type |
| Body Size Matching | Liver size must match (especially in pediatric or small adults) |
| Medical Urgency | Acute liver failure or ICU admission may push up priority |
| Hospital/City Quota System | Acute liver failure or ICU admission may push up the priority |
⚠️ Note: Priority may vary slightly depending on the state rules and hospital policies, but the MELD score is the backbone in most systems.
🏥 Why Staying Near the Transplant Hospital Is Essential
Being on the liver transplant waitlist for a cadaver organ can feel like waiting in limbo. But proximity to your transplant centre isn’t just a convenience; it is a life-saving strategy.
📍 Reasons to Stay Close to the Transplant Centre:
✅ Urgent Call Window: When a suitable liver becomes available, you may have only 6–12 hours to reach the hospital. Patients living far away may miss the chance altogether.
✅ Ongoing Reassessments:
While on the waitlist, regular reassessments and repeat testing may be required, especially if your previous tests are older than 3–6 months or your health status changes.
✅ Better Pre-Transplant Optimisation:
Living close to the hospital allows timely management of:
- Infections
- Malnutrition
- Fluid overload
- Coagulation abnormalities
Being optimised improves both surgical outcomes and survival.
✅ Timely Communication with the Transplant Coordinator:
Your transplant team needs to know where you are, how fast you can reach, and whether you’re still eligible. Staying nearby allows seamless communication.
✅ Shifting States? No Problem.
Even if you’re from another state, relocating temporarily near the transplant centre is worth considering. Many families find rented accommodation or hospital-provided facilities nearby during this period.
🚫 Despite Preparation, Not All Patients Get an Organ
Unfortunately, due to the shortage of donor livers, especially blood group O (universal donor), some patients may wait for months or even years. In many cases, patients deteriorate or pass away before an organ becomes available.
This is heartbreaking but real.
💡 When Living Donation May Be a Better Option
Living Donor Liver Transplant (LDLT) is a well-established alternative with better outcomes. Whenever feasible:
- Doctors counsel the family to consider living donation
- Planned surgery can be performed at the earliest sign of recipient readiness
- Survival outcomes are significantly better due to optimal timing
Frequently Asked Questions
How long does a patient wait for a liver transplant in India?
It depends on several factors, especially blood group and MELD score.
- For blood group O, the wait is usually longer
- Some patients wait months to years
- Sadly, many don’t survive the wait
That’s why staying close to the hospital and exploring living donation options are so important.
Who is eligible to donate their liver in life?
- Healthy persons between the ages of 18 and 60 who have a suitable blood type and no noteworthy medical history are usually living liver donors.
- They undergo rigorous medical and psychological evaluations to ensure suitability.
What hazards does the donor face?
- Infection, rare incidences of liver failure, and surgical complications are among the hazards associated with liver donation, despite its general safety.
- Excellent long-term health outcomes are typically achieved, but donors need to be mindful of any possible hazards.
How much time does it take for the liver of the donor to heal?
Immediately following surgery, the liver starts to recover. In most donors, within 2-4 weeks, liver function returns to normal. Liver volume: returns after three months to 90–95% of its initial level. Liver size: Regains almost its entire volume within a year.
How successful is LDLT?
- LDLT has a high success rate, with recipients surviving for more than 90% of the year.
- Success is contingent on a number of variables, including the recipient’s general health and compliance with post-transplant treatment.
Can a donor resume their regular life after donating?
Indeed, the majority of donors resume their regular activities in two to three months and go on to lead healthy lives free from long-term issues.
How much does a liver transplant cost in India in 2025?
Costs vary, but here’s an approximate breakdown:
| Type of Transplant | Estimated Cost (INR) |
|---|---|
| LDLT (Adult) | ₹19–24 Lakhs |
| LDLT (Pediatric) | ₹14–16 Lakhs |
| DDLT (Deceased) | ₹35–40 Lakhs |
💡 Always verify with your hospital — this is just an estimate.
Is a liver transplant cheaper in India than abroad?
Yes. Compared to the US and Europe, India offers world-class liver transplant services at a significantly lower cost, often 1/5th of the price.
Which hospital is best for liver transplant in India?
Many centres across India, especially in Delhi NCR, Mumbai, Chennai, and Hyderabad, offer excellent outcomes. It’s important to choose a transplant program with experienced teams, high case volume, and transparent outcomes.
Why do doctors recommend a living donor even if I’m on the waitlist?
Because cadaver organs are scarce, and delays reduce survival.
Living donation allows:
- Timely surgery when the patient is optimized
- Reduced risk of sudden deterioration
- Better long-term outcomes
Conclusion
Living donor liver transplant is an incredible medical breakthrough. It gives patients with advanced liver disease hope.
Comprehensive pre-transplant counselling for the patient and donor is necessary for the process to be successful. By addressing psychological, medical, and ethical issues, the transplant team makes sure that everyone is ready for the journey.
🧩 Counselling Is Tailored — Not Templated
Every transplant journey is different. Some families are well-informed, others are overwhelmed.
Some donors are enthusiastic, others are anxious. We listen, we guide, we customise.
Pre-liver transplant counselling is not a formality. It’s the foundation of trust, safety, and shared decision-making — and it continues until the moment the patient enters the OR.
Share your questions in the comments section or consult a transplant specialist for personalised advice!
📘 More Help for Your Liver Health Journey
🆓 Free eBooks by Dr. Tanuja Mallik:
- Know Your Medicine – Understand key post-transplant medications
- Best Foods for Liver Health – What to eat (and avoid) for optimal liver care
💬 Got a liver issue or recovering from transplant?
Book a 1-on-1 Online Consultation for personalised recovery & guidance.
🔗 Access all resources here: linktr.ee/drtanujamallik
Very informative and comprehensive.
“I really appreciate you taking the time to share your thoughts.”
Thank you so much Dr Puneet Dargan 🙂