Introduction
“My mother’s scan says the liver is cirrhotic.”
“There’s fluid in the abdomen—what does it mean?”
“Is cirrhosis curable? Can we reverse it?”
These are the kinds of messages I receive every week from patients and caregivers. Behind each one is anxiety, confusion, and often, a race against time.
Cirrhosis of the liver is a chronic and progressive disease marked by liver fibrosis—scarring that disrupts the organ’s structure and function. As the liver hardens and shrinks, its ability to perform vital tasks like detoxification, protein synthesis, and fat digestion deteriorates. The disease is often silent in its early stages, only revealing itself when significant, sometimes irreversible damage has already occurred.
As a liver transplant anaesthetist, I’ve seen too many lives altered or lost, not just to the disease, but to the lack of timely awareness. Most people don’t realise that cirrhosis is not reversible. While we can treat the complications, the only definitive solution in advanced stages is a liver transplant.
The earlier families understand this, the better. Timely awareness allows for:
- Exploring family donor options
- Preparing for deceased donor liver transplant (DDLT) listing
- Arranging finances in time
- Gaining emotional and mental readiness
This preparation can be the difference between a planned, supported transplant and a rushed emergency that leaves little room for choice or stability.
That’s exactly why I created this blog. Not just as a doctor, but as someone who has seen what clarity can do. I’ve answered the most searched questions on Google about cirrhosis—from early symptoms and prognosis to transplant and treatment—to help patients and caregivers make informed, life-saving decisions. Let’s cut through the confusion, address the fears, and give cirrhosis the attention it demands—before it’s too late.
🎙️Podcast on Liver Cirrhosis
Frequently Asked Questions
🔹 What is cirrhosis of the liver?
Cirrhosis, a late stage of liver fibrosis, is brought on by a variety of liver disorders, including prolonged drinking, hepatitis, etc. Fibrosis is a sluggish, years-long scarring process that causes the liver to shrink and stiffen.
The smooth liver surface becomes lumpy due to scar tissue, which obstructs blood flow and causes portal hypertension.
🔹 What causes cirrhosis of the liver?
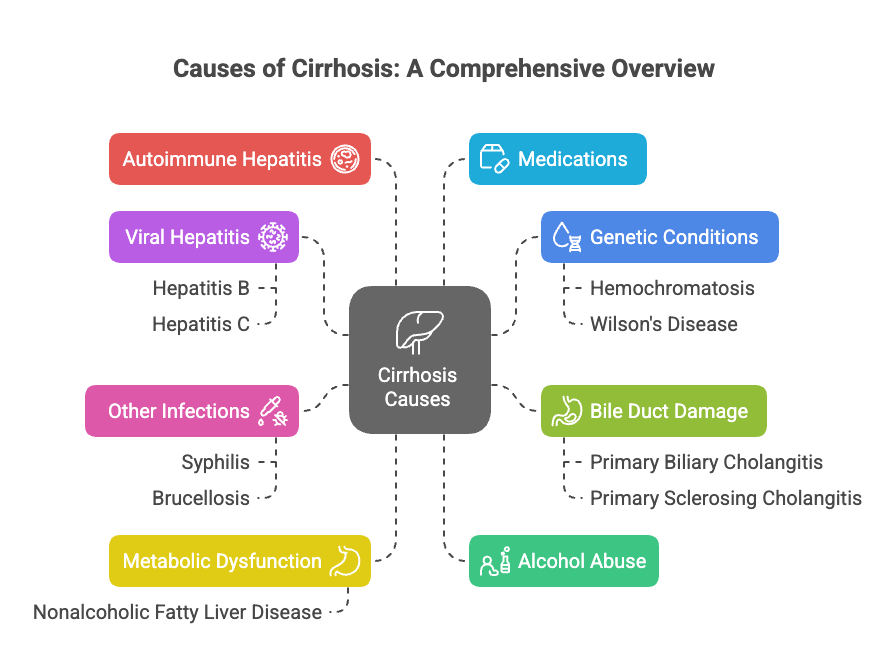
A wide range of conditions can damage the liver and result in cirrhosis. Common causes highlighted across the sources include:
- Chronic hepatitis B or C infections
- Alcoholic liver disease
- Non-alcoholic fatty liver disease (NAFLD)
- Autoimmune hepatitis
- Genetic disorders (e.g., Wilson’s disease, hemochromatosis)
- Prolonged exposure to toxins or certain drugs
- Cryptogenic (Cause Unknown)
🔹 What are the 4 stages of cirrhosis of the liver?
- Stage 1 (Compensated Cirrhosis): Mild scarring with few or no symptoms.
- Stage 2: Portal hypertension begins, with possible swelling or varices.
- Stage 3 (Decompensated): Ascites, hepatic encephalopathy, bleeding.
- Stage 4: End-stage liver disease – life-threatening complications.
🔹 Can liver cirrhosis be reversed?
Technically no
Once a liver is diagnosed with cirrhosis, it means the damage has progressed, typically stage 3 or 4 on a FibroScan. At this stage, the liver has developed permanent scarring, and unfortunately, the condition is not reversible.
Here’s what you need to understand:
- Cirrhosis is progressive, not reversible. You cannot reverse the damage, but you can slow down further progression by managing the root cause.
- For example:
- Alcohol-related liver disease: Stopping alcohol can significantly slow down the disease.
- Fatty liver (MASLD): Managing diabetes, obesity, and cholesterol can prevent worsening.
What doctors can do:
We treat the symptoms and complications, not the underlying damage.
Common complications include:
In reality, most patients with cirrhosis will eventually require a liver transplant. It may not be urgent today, but it’s wise to:
- Understand your stage
- Discuss transplant planning early
- Prepare financially and emotionally
- Keep regular follow-ups with your hepatologist
🔹 How I cured my liver cirrhosis (Real Stories vs Reality)
While some online claims say “I cured cirrhosis,” be cautious. Early-stage liver damage may improve, but true cirrhosis (Stage 3 or 4) is often irreversible. Focus on managing the cause, symptoms, and complications and preventing further damage.
🔹 Is cirrhosis a liver cancer?
No, cirrhosis is not cancer. However, cirrhosis increases your risk of developing liver cancer (Hepatocellular carcinoma).
🔹 What are the signs of end-stage cirrhosis?
Warning signs of end-stage cirrhosis include:
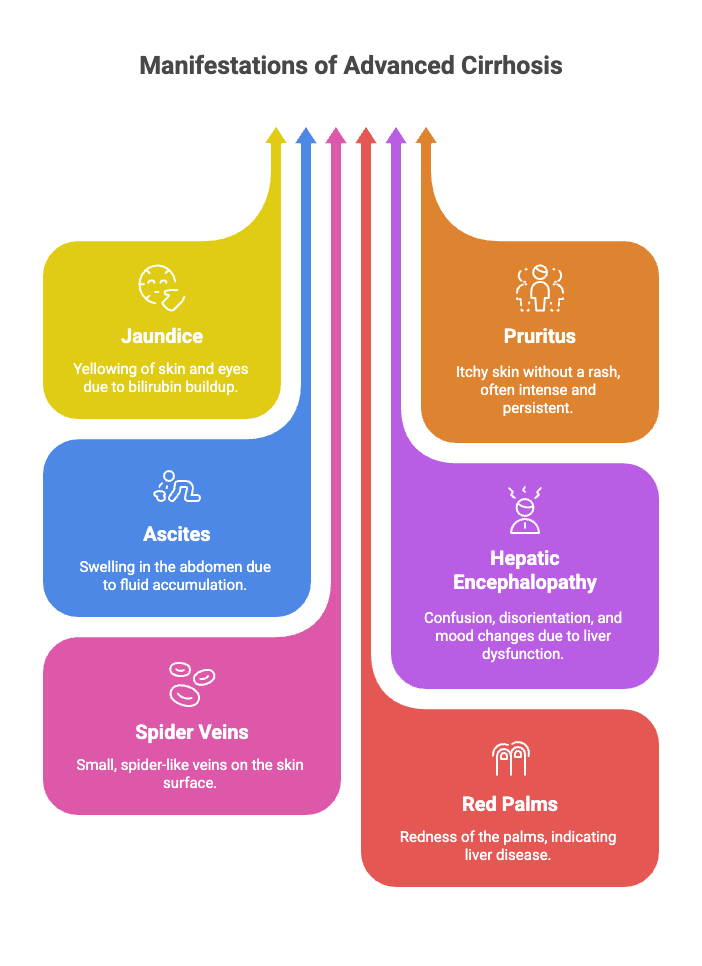
- Severe confusion (hepatic encephalopathy)
- Bleeding varices (vomiting blood)
- Ascites (fluid in the belly)
- Jaundice
- Kidney dysfunction
- Frequent infections
These require immediate medical attention.
🔹 How does cirrhosis impact life expectancy or survival?
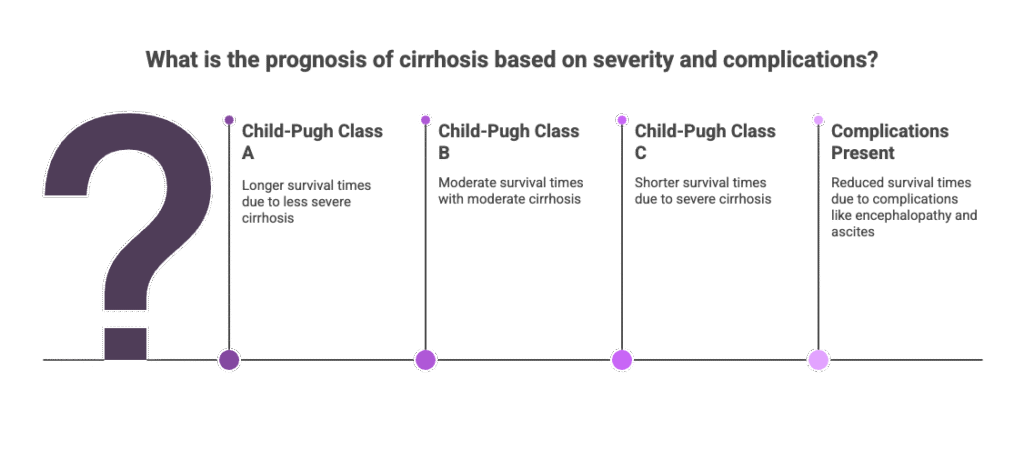
There is no one-size-fits-all answer. It depends on:
- The stage of liver damage
- The presence of complications
- The underlying cause
- The response to medical management
This varies. If untreated, especially after complications arise, cirrhosis can shorten lifespan to months or a few years. The onset of complications like hepatic encephalopathy, ascites, and hepatorenal syndrome (Kidney involvement) is associated with reduced survival times.
Survival is significantly reduced for patients with organ failures and infections. So, consult your doctor and do the needful.
🔹 What is the best treatment for liver cirrhosis?
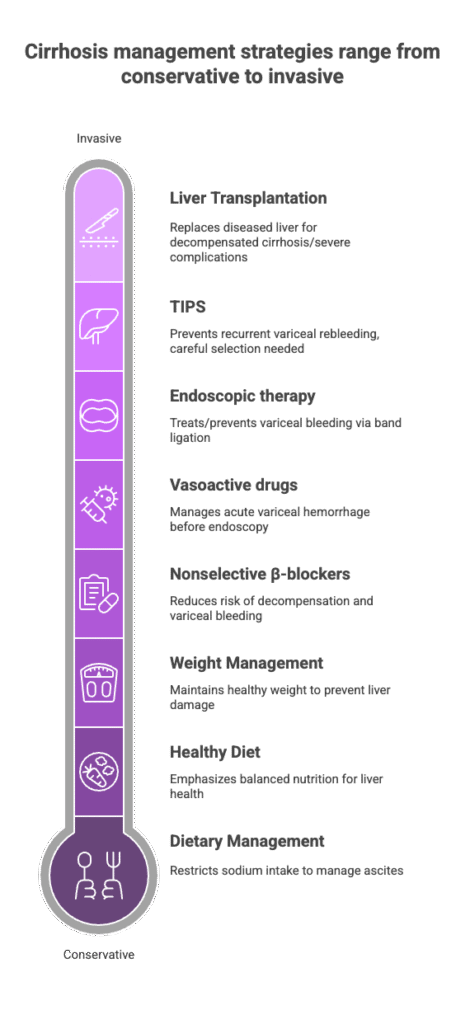
Treat the Underlying Cause: Stop alcohol use immediately. Treat hepatitis with antivirals. Manage metabolic risk factors like diabetes and obesity. Address autoimmune, genetic, or biliary diseases specifically.
Diet and Lifestyle:
To control ascites, follow a low-sodium diet (less than 2 grams per day).
Steer clear of canned, processed, and salty meals.
Sufficient consumption of protein unless otherwise advised (e.g., HE).
For MASLD/ Fatty liver disease, weight loss and consistent exercise are recommended.
Diuretics for ascites.
Rifaximin with lactulose for encephalopathy.
Beta-blockers to stop variceal haemorrhage and lower portal pressure.
Steroids or antivirals, based on the underlying reason.
Monitoring and Assistance: Frequent Endoscopy (EGD) for the screening of varices.
Every six months, AFP and imaging tests are performed for HCC surveillance.
Early management of problems such as Hepatorenal syndrome/HRS and Spontaneous bacterial peritonitis/ SBP.
TIPS: May be used to stop repeated variceal rebleeds, but because of the possibility of consequences such as hepatic encephalopathy, it is important to choose patients carefully.
Liver transplantation: Taken into consideration for patients who meet transplant criteria for HCC, recurrent problems, or decompensated cirrhosis. Prioritising candidates is aided by the MELD (Model for End-Stage Liver Disease) score.
🔹 Can you donate part of your liver to someone with cirrhosis?
Yes. In a living donor liver transplant (LDLT), a healthy person donates a portion of their liver to someone with end-stage cirrhosis. The liver regenerates in both the donor and the recipient. It’s life-saving when done at the right time.
🔹 How long can you live with cirrhosis of the liver stage 4?
On average, people may live months to a few years, depending on:
- The cause
- Response to treatment
- Availability of transplant
But every case is unique — hope and help both exist.
🔹 How is cirrhosis diagnosed?
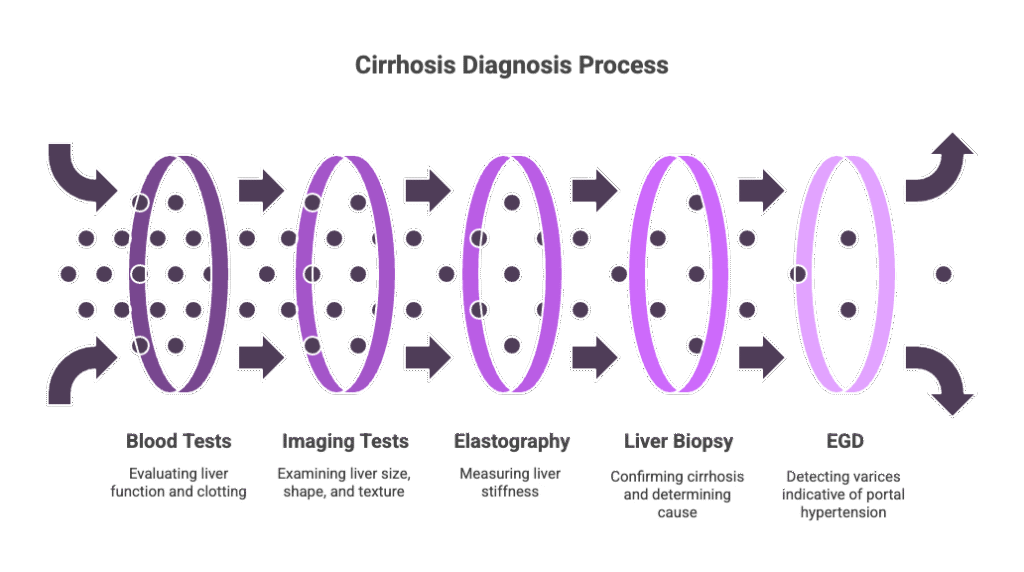
The patient’s medical history, a physical examination, and several tests are usually used to diagnose cirrhosis.
- By assessing levels of liver enzymes, proteins, and bilirubin, blood tests are used to evaluate liver function. They can also reveal decreased blood coagulation.
- The size, shape, and texture of the liver are examined using imaging procedures such as abdominal ultrasounds, CT scans and MRIs.
- Liver stiffness is measured by elastography, a unique imaging modality that uses ultrasound or MRI and corresponds with the degree of fibrosis; cirrhosis is usually confirmed if the liver stiffness is 15 kPa or more.
- A liver biopsy, which entails removing a small sample of liver tissue for laboratory analysis, is still the gold standard for identifying the origin of cirrhosis and verifying its existence, even if it is not always required.
🔹 What are the major complications of cirrhosis?
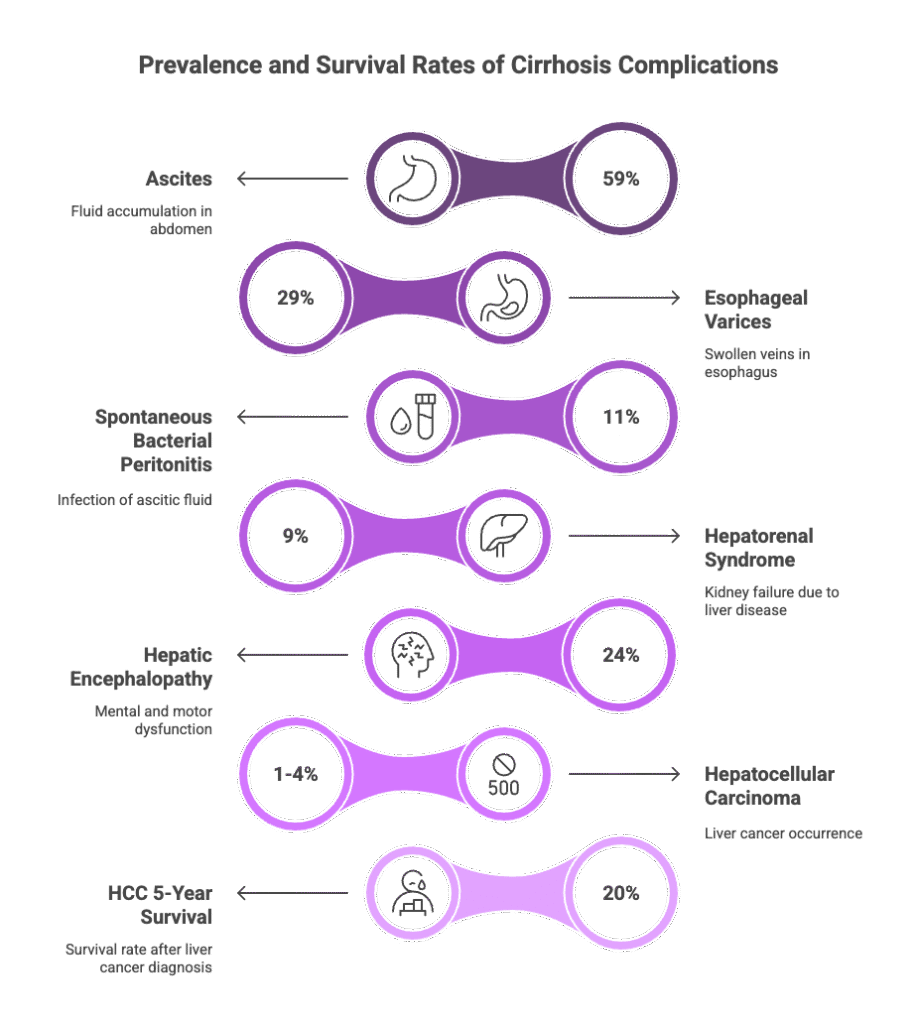
Cirrhosis can result in several complications.
- Ascites, or fluid accumulation in the abdomen;
- Hepatic encephalopathy, or brain dysfunction brought on by the liver’s incapacity to eliminate toxins.
- Variceal haemorrhage, or bleeding from enlarged blood vessels in the stomach or oesophagus as a result of portal hypertension;
- Spontaneous bacterial peritonitis, or infection of the ascites fluid.
- Hepatorenal syndrome, or kidney dysfunction, and
- Hepatocellular carcinoma, or liver cancer, is one of these conditions.
- Sexual dysfunction, pruritus, cramping in the muscles, and poor sleep are additional possible complications.
🔹How are cirrhosis patients treated for ascites?
A common complication of cirrhosis is ascites, or the buildup of fluid in the abdomen. Because too much salt exacerbates fluid accumulation, management usually starts with –
- Dietary salt restriction, usually less than 2 grams daily. Diuretics, especially loop diuretics and aldosterone antagonists, are frequently used to promote the excretion of water and salt.
- In cases of refractory ascites (ascites that don’t respond to diuretics and sodium restriction), procedures like large-volume paracentesis (removing the fluid with a needle) or the insertion of a transjugular intrahepatic portosystemic shunt (TIPS) may be necessary.
- TIPS poses the risk of complications, including hepatic encephalopathy, but it can also help decompress the portal system, enhance renal function, and lessen ascites.
🔹What is hepatic encephalopathy, and how is it treated?
Toxin buildup, especially ammonia, in the brain causes cirrhosis-related neuropsychiatric complications called hepatic encephalopathy (HE). The symptoms can include mild cognitive impairments (minimal HE), disorientation, confusion, motor dysfunction, and even coma (overt HE).
- Reducing the body’s toxin levels is the main goal of treatment for HE. One typical treatment is lactulose, a form of sugar that helps to reduce ammonia levels. Because it can lessen the amount of bacteria in the gut that produce ammonia, the antibiotic Rifaximin is also utilised.
- In certain situations, dietary protein changes might be taken into consideration, and therapies for certain symptoms, like cramping in the muscles or poor sleep, might also be used. The best course of treatment in severe or recurring cases might be liver transplantation.
🔹Can cirrhosis be prevented?
Although there is no way to reverse established cirrhosis, addressing the underlying reasons and maintaining liver health can decrease its progression.
- Avoiding alcohol intake is part of this, particularly if you have liver problems.
- Steatotic liver disease/ fatty liver disease linked to metabolic dysfunction can be avoided by eating a healthy liver diet high in fruits, vegetables, and whole grains and low in fatty and fried foods.
- Maintaining metabolic parameters like cholesterol, blood pressure, and blood sugar at the optimum level.
- Because too much body fat might harm the liver, it’s also very important to maintain a healthy weight.
- Cirrhosis can also be avoided by lowering the risk of viral hepatitis B and C through safe practices (avoid sharing needles and unprotected sex) and taking into account hepatitis immunisations.
To explore the medications commonly used in treating hepatic encephalopathy and ascites in liver disease patients, please refer to our detailed guide in the blog post Know Your Medicine.
📌 Final Word:
Cirrhosis is not the end — it’s your body’s wake-up call.
Ignoring early signs of liver disease leads to irreversible damage. But with timely detection, the right treatment, and lifestyle changes, you can slow down the disease progression to some extent. In most cases, it is impossible to completely reverse the liver damage. Limiting additional damage and preventing liver failure can be achieved by treating the underlying cause of cirrhosis and managing its consequences. — or prevent complications.
The most powerful step you can take is awareness. Understand the severity of your condition. Talk openly with your hepatologist or physician. Get a clear roadmap of what lies ahead. Know the symptoms: jaundice, abdominal fluid (ascites), bleeding, mental confusion, and reduced urine output — and act early.
If you or a loved one is already in the advanced stage, this is the time to act with courage and clarity. Start exploring transplant options. Talk to your transplant team. Discuss the possibility of a living donor from your family, or consider getting listed for a deceased donor liver transplant.
Change your lifestyle — stop alcohol, eat liver-friendly food, and stick to your follow-ups. Give yourself and your family the chance to access the right care, emotional support, and education.
Fear isn’t the solution. Awareness is.
Many lives have been saved through liver transplants, and many are living healthy, normal lives after it.
You can be one of them. You deserve a second chance.
Remember this: Every action you take today has the potential to alter the course of tomorrow, whether you’re standing by someone you care about or battling for yourself.
💡 Stay informed. Stay strong. And remember — you are not alone on this path.
👉 Want to get a customised recovery roadmap?
🌿 Book a Online Consultation with Dr. Tanuja Mallik
For personalised guidance, you can book a one-on-one consultation using the secure payment link below:
👉 Click here to make your payment
Once your payment is confirmed, please choose your convenient time for the consultation:
📅 Schedule your appointment via Calendly
After booking, we can connect via WhatsApp or Zoom — whichever is more comfortable for you.
💬 Have questions before you book? Feel free to reach out! I’m here to help.
Warm regards,
Dr. Tanuja Mallik
