Liver transplantation is a life-saving procedure for patients with end-stage liver disease or acute liver failure. However, the significance of liver transplant anaesthesia in ensuring a favourable outcome is just as crucial as the surgery itself. The success of the transplant largely depends on the careful management of anaesthesia, which is tailored to the patient’s unique needs.
🩺 A Quiet Conversation Before the Storm
👩⚕️ I walked into the pre-op room that morning. The air was still, yet thick with silent thoughts. Kavita sat on the edge of her hospital bed — young, brave, yet unsure.
👧 Kavita: “Will I wake up after surgery, doctor? Will I be okay?”
👩⚕️ Me: I smiled gently, placing a reassuring hand on her shoulder. “Yes, Kavita. You’ll be awake right after surgery. We’ll keep you pain-free and completely comfortable.”
She looked down for a second, then raised her eyes again.
👧 Kavita: “What about my father?”
👩⚕️ Me: “We’ll take care of him too. He’s stable and ready. Trust us — we’ll do our very best.”
👩⚕️ I then walked over to Ram Avatar’s room — her father, the recipient. He looked at me with quiet eyes, holding more fear than words.
👴 Ram Avatar: “Doctor… Will I be fine? Will I make it through?”
👩⚕️ Me: “You’re doing well. Your labs look good. You’ve done your part, now let us do ours. We’ll keep you on the ventilator tonight, and if all goes well — and we’re hopeful it will — we’ll wake you up tomorrow morning.”
I paused and added what I knew would be his next worry.
👩⚕️ Me: “Your daughter will be fine. We’ll wake her up right after surgery. She’ll be smiling — and she’ll be right there in the same ICU with you. You’ll see her there.”
Two rooms. One surgery. A bond stronger than fear. And in that quiet pre-op moment — a promise of healing, twice over.
During the procedure, liver transplant anaesthesia not only keeps the patient safely unconscious and pain-free but also ensures stable vital signs, such as blood pressure and oxygen levels, throughout the complex surgery. This is especially important as patients undergoing liver transplants often face additional risks due to compromised liver function. In this blog, we will break down the fundamentals of liver transplant anaesthesia in plain language, allowing you to better appreciate its significance and understand the intricate details that make it an essential part of the transplant journey.
What is the purpose of Liver Transplant Anaesthesia?
Liver Transplant Anaesthesia is a highly specialised and critical component of liver transplant surgery. It ensures the patient’s safety, comfort, and stability throughout the entire surgical process. This type of anaesthesia is tailored to meet the specific needs of liver transplant patients, who often have complex medical histories and compromised liver functions. The purpose of liver transplant anaesthesia is not only to keep the patient pain-free and unconscious during the procedure but also to help maintain vital functions in a stable and controlled manner, minimising the risks associated with the surgery.
Why is Anaesthesia Challenging in Liver Transplants?
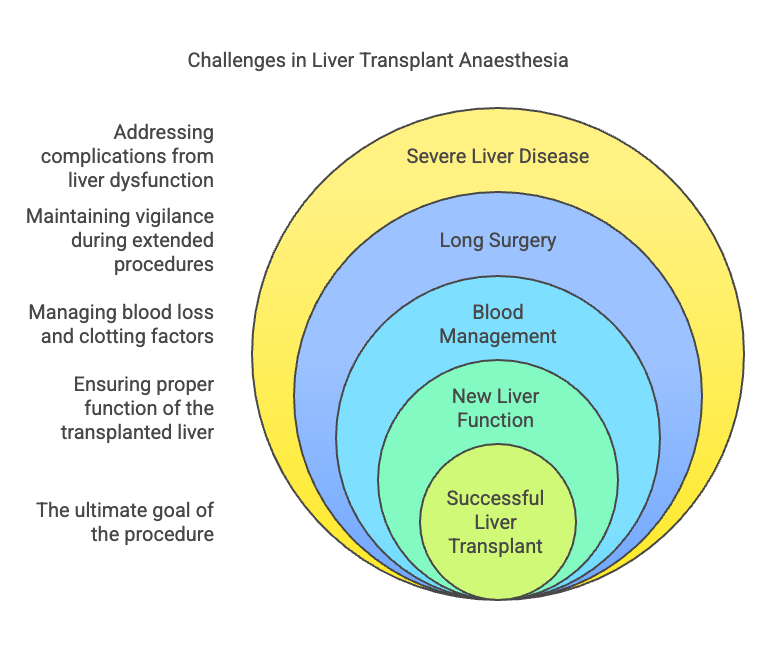
Liver transplant surgery is one of the most difficult medical procedures, and the anaesthesia required for it is just as challenging. The reason is as follows:
- Severe Liver Disease: Patients undergoing liver transplants often have severe liver disease, which complicates the anaesthesia process. Liver disease frequently leads to dysfunction in multiple organ systems, making anaesthesia management more difficult. Some common challenges that arise include:
- Fluid Imbalances: The liver plays a key role in fluid and electrolyte balance. When the liver is failing, it can cause issues such as ascites (fluid accumulation in the abdomen), leading to imbalances in the body’s sodium and fluid levels. The anaesthesiologist must be skilled in adjusting fluid management to maintain normal blood volume and pressure.
- Bleeding Issues: Severe liver disease can impair the body’s ability to form blood clots, leading to increased bleeding risks. The anaesthesiologist must be vigilant in managing blood loss, which may involve administering blood products like plasma or platelets and using medications to help promote clotting.
- Altered Sensory Perception: Patients with liver disease may also experience altered mental status, such as confusion or disorientation (hepatic encephalopathy), due to the buildup of toxins in the body that the liver can no longer filter. The anaesthesiologist needs to account for these altered states and adjust medication doses accordingly.
- Low Blood Pressure and Urine Output: Liver disease can also affect the kidneys, resulting in low blood pressure (hypotension) and reduced or absent urine output (oliguria or anuria). This makes it even more challenging to regulate the patient’s vital signs and ensure that the organs are receiving adequate blood flow during surgery.
- Long Surgery: Liver transplant surgery is typically a long and complex procedure, often lasting anywhere from 6 to 12 hours, depending on the complexity of the case. During this extended period, the anaesthesiologist must maintain a high level of vigilance and continuously monitor the patient’s condition. The need for frequent adjustments to anaesthesia and vital signs management is essential, as the patient’s condition may change throughout the surgery.
- Monitoring Vital Signs: For many hours, the anaesthesiologist must keep track of the patient’s heart rate, blood pressure, oxygen levels, and other vital signs. Small changes in these parameters can lead to significant complications during surgery, so quick responses are necessary to keep the patient stable.
- Adjusting Anaesthesia: As the surgery progresses, the anaesthesiologist must continuously adjust the anaesthesia levels to match the patient’s needs, especially as the body responds to surgery, blood loss, and other variables. Fatigue and stress on the body can also require adjustments to ensure that the anaesthesia is neither too deep nor too light.
- Blood transfusions and Clotting factors management: One of the major challenges in liver transplant anaesthesia is managing significant blood loss during the surgery. Liver transplant surgeries often involve substantial blood loss due to the complexity of removing the diseased liver and performing the transplant. The anaesthesiologist’s role in managing blood transfusions and clotting factors is crucial:
- Blood Loss Management: Given the large amounts of blood that may be lost during the surgery, blood transfusions are often necessary. The anaesthesiologist must coordinate with the surgical team to determine when and how much blood to administer to maintain an optimal blood volume and pressure.
- Clotting Factors: The liver is responsible for producing many of the body’s clotting factors. When the liver is diseased, clotting may be impaired, increasing the risk of uncontrolled bleeding. The anaesthesiologist must administer clotting agents and blood products like fresh frozen plasma (FFP) or cryoprecipitate to prevent excessive bleeding during surgery.
- New Liver Function: Once the new liver is transplanted into the patient, the anaesthesiologist plays an important role in ensuring its proper function. The transplanted liver must be assessed immediately to ensure that it is receiving adequate blood flow and oxygenation.
- Blood Flow and Oxygenation: After transplantation, the new liver may be more susceptible to ischemia (lack of oxygen) due to the surgical procedure. The anaesthesiologist is responsible for managing the patient’s circulation to ensure that the liver receives adequate blood flow and oxygen to support its function.
- Ensuring Graft Function: The anaesthesiologist must also watch for any signs of liver graft dysfunction, such as poor bile production or signs of liver rejection, and communicate with the surgical team to address any concerns that may arise. This often includes closely monitoring liver enzymes, blood gas levels, and other indicators of liver function.
- A High-Stakes and Complex Task
- Liver transplant anaesthesia presents a unique set of challenges that require a high level of expertise, precision, and constant vigilance. From managing the complexities of severe liver disease to ensuring proper blood flow to the new liver, the anaesthesiologist plays a crucial role in the success of the procedure. The need for continuous adjustments, monitoring, and collaboration with the surgical team highlights the importance of anaesthesia in liver transplant surgery. While the procedure itself is long and arduous, the anaesthesiologist’s skill in managing the numerous variables that come with liver transplant anaesthesia can make the difference between a successful transplant and a life-threatening complication.
What Does the Anaesthesiologist Do?
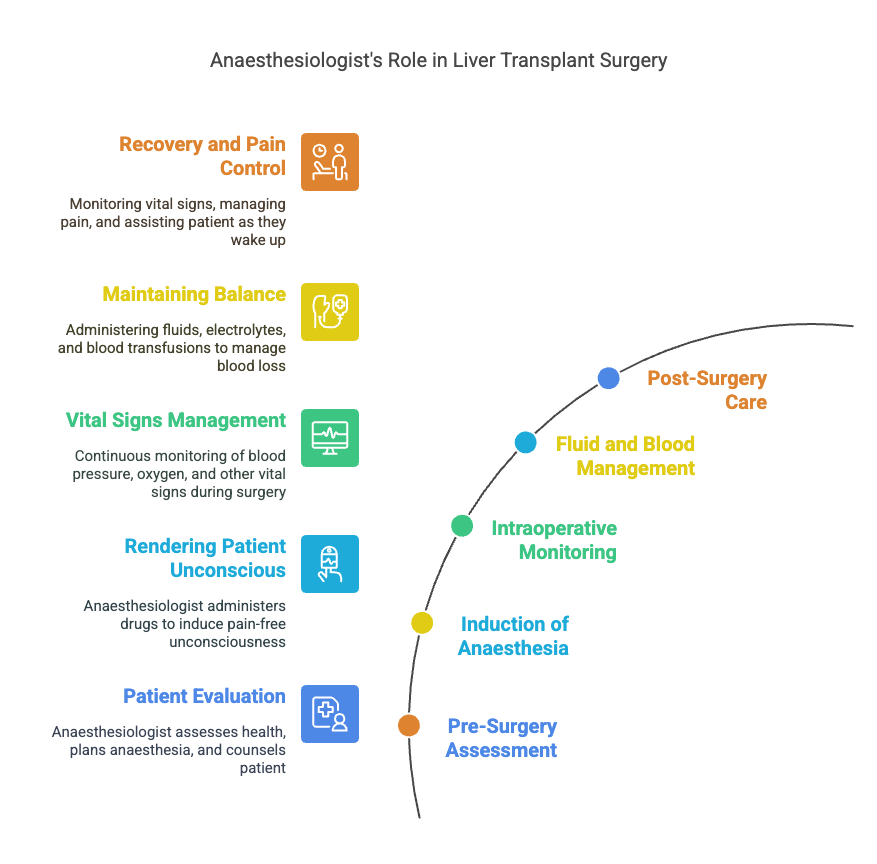
In liver transplant surgery, the anaesthesiologist plays a vital and multi-faceted role that can be likened to being the patient’s “guardian angel.” Their expertise and presence are essential throughout the entire procedure, from pre-surgery preparations to post-surgery recovery. Here’s a detailed look at the key responsibilities of an anaesthesiologist during a liver transplant:
1. Pre-Surgery Assessment and Pre-Transplant Counselling
Before the transplant begins, the anaesthesiologist’s job is to thoroughly evaluate the patient’s overall health and identify any factors that could complicate the anaesthesia process. This includes:
- Assessing Vital Organ Functions: The anaesthesiologist examines the patient’s heart, lungs, liver, kidneys, brain, and clotting factors to assess their ability to handle the stresses of surgery and anaesthesia. In liver transplant patients, this is particularly crucial because they often have multiple organ dysfunctions.
- Tailoring the Anaesthesia Plan: Based on the assessment, the anaesthesiologist customises the anaesthesia strategy to meet the specific needs of the patient. This may involve adjusting the anaesthesia drugs and dosages to account for any existing conditions, such as liver or kidney dysfunction.
- Pre-Transplant Counselling: Part of the anaesthesiologist’s responsibility is to ensure the patient is fully informed and emotionally prepared for the surgery. They provide clear, detailed explanations about the anaesthesia process and what to expect. This helps lower the patient’s anxiety levels and sets realistic expectations for the procedure and recovery.
- Obtaining Consent: The anaesthesiologist also takes the time to explain the risks associated with anaesthesia, including any specific concerns related to liver transplant surgery. They ensure the patient provides informed consent, usually in the form of written or video consent, so the patient is well aware of what will happen during surgery.
2. Inducing Anaesthesia
Once the patient is ready for the surgery, the anaesthesiologist is responsible for rendering the patient unconscious and pain-free. This involves:
- Administering Anaesthetic Drugs: The anaesthesiologist uses a combination of intravenous drugs and gases to induce anaesthesia. These drugs are carefully chosen based on the patient’s medical history and the demands of liver transplant surgery. The goal is to make the patient completely unconscious, pain-free, and relaxed, while maintaining stable vital signs.
- Managing Anaesthesia Levels: During induction, the anaesthesiologist carefully monitors the patient’s response to the drugs and adjusts the dosages as needed. This ensures that the patient is fully anaesthetised and the surgical team can perform the procedure without the patient experiencing any pain or distress.
3. Vital Signs Monitoring
Throughout the surgery, the anaesthesiologist has continuous oversight of the patient’s vital signs to ensure their safety. This is especially important in liver transplant surgeries, where blood pressure, oxygenation, and other vital parameters can fluctuate significantly. Key responsibilities include:
- Monitoring Blood Pressure and Heart Rate: The anaesthesiologist must track the patient’s blood pressure and heart rate closely, making adjustments as necessary to keep the body’s circulatory system stable throughout the procedure. If there are significant drops in blood pressure, immediate action is required to correct it.
- Oxygen Levels and Ventilation: Ensuring that the patient receives adequate oxygen during the procedure is critical, especially since the liver transplant can involve periods of low blood pressure and reduced oxygenation. The anaesthesiologist monitors oxygen saturation levels and adjusts ventilation support as needed.
- Keeping Track of Other Vital Signs: In addition to blood pressure and oxygen saturation, the anaesthesiologist also tracks other important parameters, such as body temperature and electrolyte levels, ensuring that the body remains stable throughout the lengthy surgery.
4. Managing Fluids and Blood Loss
Blood loss is a common concern during liver transplant surgery due to the complexity of the procedure. The anaesthesiologist plays a crucial role in managing fluid and blood replacement:
- Administering Fluids and Electrolytes: During the surgery, the anaesthesiologist ensures that the patient receives the appropriate amount of intravenous fluids to maintain hydration, support circulation, and restore any lost blood volume. This is essential, as the liver plays a key role in fluid balance, and its dysfunction can lead to complications like low blood pressure or organ failure.
- Blood Transfusions: Liver transplant surgeries often require significant blood transfusions due to blood loss during the procedure. The anaesthesiologist coordinates with the surgical team to manage blood products and ensure that the patient receives the right amount of transfusions based on their individual needs.
- Clotting Factor Management: Since liver disease often impairs the body’s ability to clot, the anaesthesiologist also monitors clotting factors and administers medications or blood products like fresh frozen plasma (FFP) to prevent excessive bleeding during surgery.
5. Surgery Care and Post-Surgery Monitoring
Once the liver transplant surgery is complete, the anaesthesiologist’s job is not over. They continue to monitor the patient as they awaken from anaesthesia and assist with pain management and recovery:
- Pain Management: After surgery, the anaesthesiologist is responsible for managing the patient’s pain. This involves carefully administering analgesic medications and adjusting the dosage to ensure the patient remains comfortable without compromising their recovery.
- Monitoring Post-Surgery Vital Signs: In the immediate postoperative period, the anaesthesiologist continues to monitor the patient’s vital signs to ensure they stabilise and recover. This may involve monitoring oxygenation, blood pressure, kidney function, and other key parameters to prevent complications such as bleeding, infection, or organ rejection.
- Assisting with Recovery: As the patient begins to wake up from the anaesthesia, the anaesthesiologist ensures they are comfortable and that their vital signs are stable. If necessary, the anaesthesiologist helps manage sedation levels to avoid any distress as the patient regains consciousness.
The Anaesthesiologist’s Essential Role
The role of the anaesthesiologist in liver transplant surgery is integral to the patient’s safety and the procedure’s success. From the initial pre-surgery assessments to the meticulous management of anaesthesia during surgery and post-operative recovery, the anaesthesiologist is there every step of the way, ensuring the patient remains stable, pain-free, and safe. Their expertise helps mitigate the risks associated with liver transplantation, which is a complex and high-stakes procedure. With the anaesthesiologist’s careful attention to detail, the likelihood of a successful outcome is significantly increased, making them an indispensable part of the liver transplant team.
Major Challenges During Liver Transplant Anaesthesia
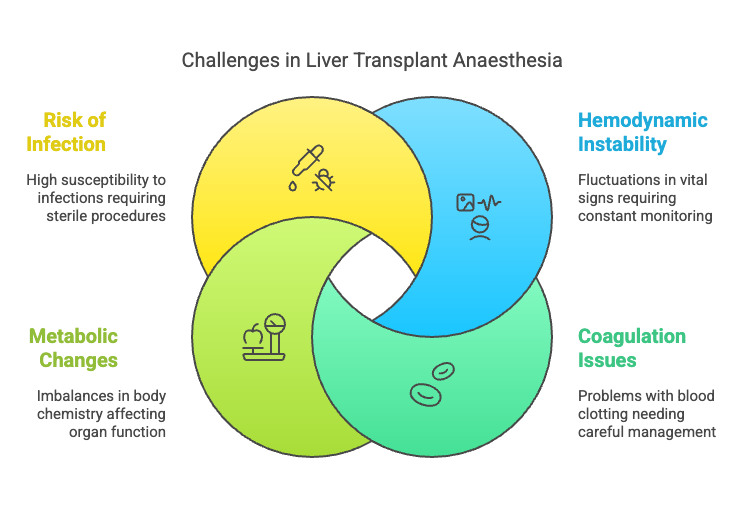
Liver transplant surgery is a highly complex and delicate procedure that presents several challenges for the anaesthesiologist. The role of anaesthesia in these surgeries goes beyond just sedation and pain management; it also involves careful monitoring and management of the patient’s physiological status, which can fluctuate dramatically due to the patient’s underlying liver disease and the nature of the surgery itself. Let’s delve into the major challenges faced during liver transplant anaesthesia:
1. Hemodynamic Instability
What is it? Hemodynamic instability refers to significant fluctuations in blood pressure, heart rate, and oxygen saturation during the surgical procedure. These fluctuations can occur suddenly due to blood loss, blood transfusions, or other factors related to the liver transplant process.
Why is it a challenge? The liver plays a central role in maintaining fluid and electrolyte balance, blood pressure regulation, and metabolic function. In patients with liver failure, these regulatory systems are often compromised. During the transplant, there may be sudden drops in blood pressure (hypotension) or changes in heart rate, especially when the diseased liver is removed and the new liver is transplanted. This can lead to hemodynamic instability, which requires constant monitoring and interventions from the anaesthesiologist.
What does the anaesthesiologist do? The anaesthesiologist must be vigilant in monitoring vital signs and ready to intervene if necessary. This often involves the administration of medications (e.g., vasopressors or inotropes) to stabilise blood pressure, fluids to maintain circulation, and other supportive measures to prevent any sudden drops in oxygen levels or heart rate. Additionally, close monitoring of the heart’s electrical activity is crucial to detect any abnormal rhythms that might arise from the instability.
How do they manage it?
- Continuous infusion of vasopressors, fluids, and medications as needed to stabilise blood pressure.
- Close monitoring of cardiac output and using invasive monitoring, like arterial lines, to track real-time hemodynamic changes.
- Use of advanced equipment to support respiratory function (e.g., mechanical ventilation) in case of oxygenation challenges.
2. Coagulation Issues
What is it? Coagulation issues refer to problems with the blood’s ability to form clots, which is critical to stop bleeding during surgery. Liver disease, particularly cirrhosis, can severely affect the body’s ability to produce clotting factors, which are proteins in the blood that help form clots to prevent excessive bleeding.
Why is it a challenge? The liver is responsible for producing clotting factors, so when it is diseased or dysfunctional, the body’s ability to stop bleeding can be severely impaired. During liver transplant surgery, there is often significant blood loss due to the complexity of the procedure, including the removal of the old liver and connection of the new one. In such a high-risk environment, managing bleeding and ensuring proper clotting is crucial to avoid life-threatening complications.
What does the anaesthesiologist do? Anaesthesiologists need to closely monitor coagulation levels during the surgery and intervene when necessary. They must be prepared to administer blood products like fresh frozen plasma (FFP), platelets, and clotting factors to maintain the patient’s ability to form blood clots.
How do they manage it?
- During liver transplant anaesthesia, the management of coagulation is paramount to minimise the risk of bleeding complications and ensure the patient’s safety. Today, the focus has shifted primarily to INR (International Normalised Ratio) and viscoelastic testing using TEG (Thromboelastography) or ROTEM (Rotational Thromboelastometry).
- Administering blood products such as FFP, platelets, or clotting factor concentrates to correct deficiencies.
- Using medications that enhance clotting or minimise excessive bleeding, such as antifibrinolytic drugs.
3. Metabolic Changes
What is it? Metabolic changes refer to imbalances in the body’s normal chemical and electrical processes, which can affect vital organs. These imbalances can include electrolyte disturbances (e.g., sodium, potassium, calcium) and changes in blood sugar levels (hypoglycemia or hyperglycemia), especially during the early stages of liver function recovery after transplantation.
Why is it a challenge? The new liver may take some time to begin functioning properly, which can result in delayed clearance of toxins and metabolic products from the body. During this transition period, the patient may experience abnormal levels of electrolytes, blood sugars, and other metabolic markers. These changes can affect the patient’s cardiac function, kidney function, and overall stability during and after surgery.
What does the anaesthesiologist do? Anaesthesiologists must monitor electrolyte levels and adjust fluid management to keep the patient stable. Blood sugar levels, in particular, need careful management, as fluctuations can lead to complications such as low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia), both of which can impair the patient’s recovery and increase the risk of infections and other issues.
How do they manage it?
- Regular blood tests to monitor electrolytes, Blood gas analysis and glucose levels.
- Administering insulin or glucose infusions to maintain blood sugar levels within a safe range.
- Using medications to correct electrolyte imbalances (e.g., potassium replacement or calcium gluconate).
- Adjusting fluid therapy based on the patient’s metabolic needs and changes in organ function.
4. Risk of Infection and Sterile Procedures
What is it? Infection risk is high in liver transplant patients due to their compromised immune systems, which result from both the underlying liver disease and the immunosuppressive medications required after the transplant to prevent organ rejection.
Why is it a challenge? During liver transplant surgery, sterile technique is paramount to reduce the risk of infection. Contamination can lead to serious complications like sepsis, which can be life-threatening. Additionally, infections may complicate the healing process and delay the recovery of the transplanted liver, increasing the overall risk for the patient.
What does the anaesthesiologist do? The anaesthesiologist must work in close collaboration with the surgical team to ensure that strict sterile procedures are followed throughout the surgery. They also help manage antibiotic prophylaxis, ensuring the patient receives the appropriate antibiotics before, during, and after the procedure to minimise infection risk.
How do they manage it?
- Administration of prophylactic antibiotics before surgery and during the procedure reduces the risk of infection.
- Ensuring proper sterile techniques during the insertion of IV lines, intubation, and during the operation itself.
- Close monitoring for signs of infection after surgery, including using antibiotics as necessary to prevent infection from setting in.
Overcoming Challenges in Liver Transplant Anaesthesia
Liver transplant anaesthesia is a challenging and highly specialised field that requires the anaesthesiologist to manage multiple risks simultaneously. From maintaining hemodynamic stability to managing blood coagulation, metabolic changes, and infection control, anaesthesiologists play a crucial role in ensuring the safety and success of the transplant. Their ability to respond quickly to fluctuations in the patient’s condition and provide optimal care throughout the procedure is vital to a positive outcome. By understanding and addressing these challenges, the anaesthesiologist helps provide the best possible care for liver transplant patients, giving them the best chance at a successful recovery.
What Are the Differences in Anaesthesia for Liver Transplants?
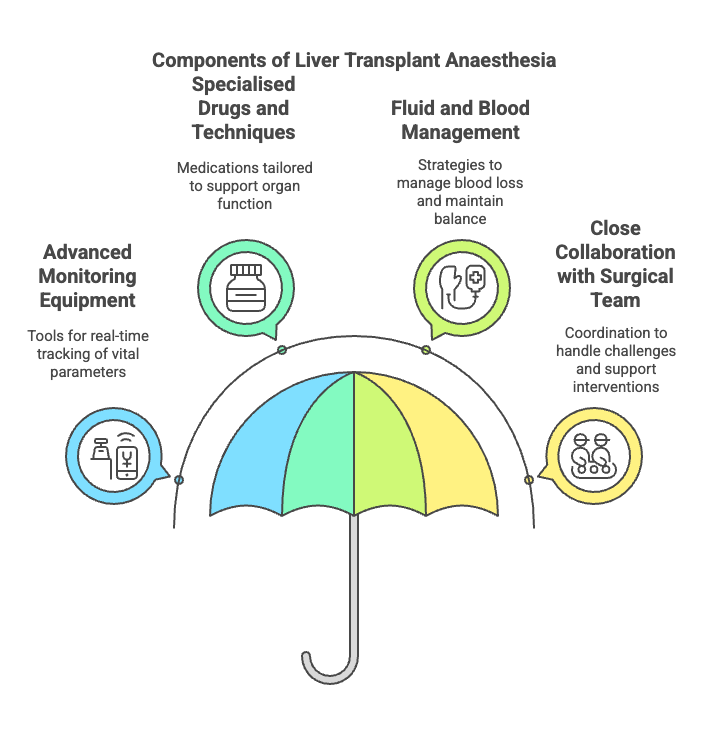
Liver transplant anaesthesia is distinct from general anaesthesia for routine surgeries due to the complexity of the procedure and the critically ill state of the patient. Here’s how liver transplant anaesthesia differs from standard surgery anaesthesia:
1. State-of-the-Art Monitoring Equipment
Liver transplant surgery requires advanced monitoring tools to assess various parameters that are crucial for the patient’s survival and recovery. These include:
- FloTrac: A minimally invasive device that continuously monitors cardiac output and other hemodynamic parameters, helping anaesthesiologists track cardiac function in real-time.
- Swan-Ganz Catheter: This catheter is used for monitoring cardiac output, central venous pressure, and pulmonary artery pressures, providing precise data on the patient’s cardiovascular status, especially when dealing with complicated cases.
- LIDCO: A non-invasive cardiac output monitor that helps assess the heart’s ability to pump blood during surgery, allowing for fluid and blood volume adjustments when needed.
These advanced technologies allow for continuous, real-time tracking of vital parameters like heart function, oxygenation, and blood pressure, which are critical during a liver transplant.
2. Specialised Drugs and Techniques
Liver transplant anaesthesia requires specific drugs to support organ function and maintain blood pressure during the prolonged surgery. These medications are tailored to the patient’s unique needs, particularly when the liver’s function is compromised due to end-stage liver disease. The anaesthesiologist must carefully balance these drugs to ensure the stability of the organs and the patient’s vital signs.
3. Fluid and Blood Management
Liver transplant surgeries often result in significant blood loss. The anaesthesiologist uses several devices and techniques to manage fluids and blood products efficiently:
- Level 1 Rapid Infuser: This device quickly warms and administers large volumes of fluids and blood products to the patient, preventing hypothermia and ensuring proper perfusion during surgery.
- Body Warmers: To maintain normothermia, body warmers are used to regulate the patient’s temperature and prevent complications like coagulopathy or infections.
Additionally, Arterial Blood Gas (ABG) analysis is done at various stages to monitor the patient’s metabolic status, including oxygen levels, blood pH, and electrolytes, which helps adjust fluid management strategies.
4. Close Collaboration with the Surgical Team
Due to the complexity of liver transplants, anaesthesiologists work in close collaboration with the surgical team. They help coordinate the timing of interventions, such as fluid boluses, blood transfusions, and medications that support liver function. The anaesthesiologist must also be prepared to handle unforeseen challenges, such as sudden blood loss or changes in the patient’s cardiovascular status, which are common in liver transplants.
The anaesthesia process for liver transplants is highly specialised and involves advanced technology, medications, and close monitoring of various physiological parameters. The anaesthesiologist must manage the patient’s cardiac function, fluid status, temperature, and respiratory needs with precision. Tools like FloTrac, Swan-Ganz catheters, LIDCO, Level 1 Rapid Infuser, and Body Warmers are essential in ensuring the patient’s stability throughout the surgery. The anaesthesiologist’s role in liver transplant anaesthesia is critical, not just in ensuring the patient is pain-free and unconscious, but in maintaining the overall stability of the patient’s organs, which directly impacts the outcome of the transplant.
The recovery process Following Liver Transplant Anaesthesia
- Following the procedure, the patient is transferred to the intensive care unit (ICU), where the anaesthetic team keeps an eye on their recuperation.
- Priority should be given to pain management and liver function support.
Why Select a Skilled Anaesthesia Group?
- Highly qualified Anaesthesiologists with backgrounds in Critical Care and Transplant Medicine are needed to provide Liver Transplant Anaesthesia.
- Their background increases the likelihood of a positive result and guarantees the patient’s safety.
Frequently Asked Questions
1. Is Liver Transplant anaesthesia dangerous?
Despite the possibility of danger, skilled Transplant Anaesthesiologists take every precaution to reduce it. The majority of patients awaken within a few hours or the next morning after Surgery.
2. Can I eat before liver transplant surgery?
No, patients are typically instructed to fast overnight before the Liver Transplantation.
3. What anaesthesia is used for a liver transplant?
Liver transplants are performed under general anaesthesia, meaning the patient is fully unconscious and pain-free throughout the surgery. A combination of inhalational agents and intravenous agents is used. These are tailored based on liver function, hemodynamics, and the stage of the surgery.
4. What anaesthesia is safe for patients with liver disease?
In patients with liver disease, anaesthetic agents are selected with caution due to impaired metabolism. The safest anaesthesia approach includes:
- Short-acting, minimal hepatic metabolism drugs (e.g., propofol, remifentanil)
- Avoidance of long-acting sedatives or muscle relaxants that depend on liver clearance
- Balanced anaesthesia with close monitoring of haemodynamics and coagulation
Anaesthesia is individualised, and continuous monitoring is critical in minimising liver stress.
5. What anaesthesia is used during liver dissection?
General anaesthesia with invasive lines, like an arterial line and a central venous line, is placed for advanced haemodynamic monitoring. It’s a major surgery with significant fluid shift and can have major blood loss. The post-surgery patient goes to the intensive care unit.
6. How does anaesthesia affect the liver?
Anaesthesia can affect liver function in several ways:
- Some agents may reduce hepatic blood flow
- Certain drugs require liver metabolism, which can strain an already compromised liver
- However, with modern techniques and drugs, anaesthesia can be managed safely even in cirrhotic or post-transplant patients when individualised care is provided.
Monitoring liver enzymes post-op is standard to detect any transient changes.
7. What is the most critical time after a liver transplant?
The first 72 hours post-transplant are considered most critical. This is when:
- Graft function is assessed
- Hemodynamic and metabolic stability are monitored
- Complications like bleeding, rejection, or primary non-function are ruled out
- Immunosuppressive drugs are initiated.
Conclusions
In order to keep the patient stable and comfortable throughout this life-altering procedure, a Liver Transplant Anaesthesiologist is an essential component of the Transplant procedure. Liver transplants are now safer and more successful than any time in history, mostly because of improvements in medical research and the skill of the Anaesthesia teams. You can be confident that the Anaesthesia team will be there to support you or your loved one throughout every step of the liver transplant preparation, surgery, and postoperative management in the ICU.
By understanding the role of Anaesthesia in Liver Transplant, you can appreciate the incredible teamwork and expertise that goes into saving lives.
💚 Ready to Understand the Journey Better?
Whether you’re a donor, recipient, or caregiver — you deserve clarity, comfort, and care. Learn more, get guided support, or simply explore real stories like Kavita and Ram’s.
💬 Book a 1:1 ConsultationIf you found this blog helpful, share it with others to spread awareness about this critical aspect of liver transplantation!
About the Author
Dr. Tanuja Mallik is a liver transplant anaesthetist and critical care specialist with years of experience in managing complex transplant cases.
Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider for personalized guidance.

Well done . Keep it up.
Thank you:)
Looking forward to your next comment!
This is a very informative and well-explained guide on liver transplant anesthesia
Thank you so much for your acknowledgement. It’s an attempt to create awareness that how pre-transplant counselling can clarify doubts and prepare and make journey of liver transplant smooth and successful!