⚠️ “He came in drowsy, eyes yellow, liver enzymes skyrocketing… the only clue? A packet of rat poison found at home.”
Rat poison-induced liver failure is a rising, silent killer in India—often misdiagnosed until it’s too late. Knowing the early signs can save a life.
Introduction
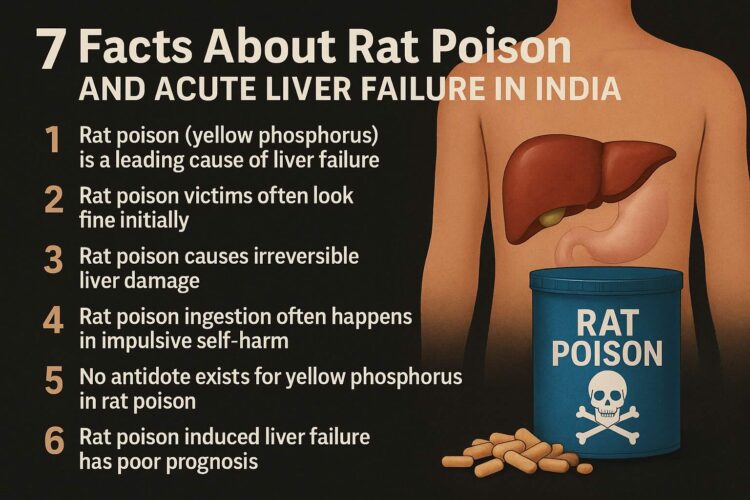
In India, rat poison—particularly that which contains yellow phosphorus—is one of the leading causes of acute liver failure. It is affordable, available, and deadly. The medical emergency known as Acute Liver Failure (ALF) is characterised by a fast decline in liver function in individuals who have never had liver illness before. Because of its distinct causes and high mortality rate (between 50% and 75%), ALF presents a special challenge in India. Rat poisoning, particularly concerning yellow phosphorus, has become a significant and expanding health concern among these causes, especially in Southern regions.
Supported by current clinical research and public health data, this blog and podcast focus on the top 7 facts regarding rodenticide exposure causing acute liver failure in India.
1. What is Acute Liver Failure (ALF) and How Is It Defined in India?
In a person without a history of liver illness, acute liver failure is characterised as the abrupt development of liver dysfunction within four weeks, accompanied by jaundice, encephalopathy (brain malfunction), and abnormal blood coagulation (prolonged prothrombin time or INR > 1.5). The Indian National Association for the Study of Liver (INASL) supports this terminology.
In contrast to Western nations where the Icterus-Encephalopathy Interval (IEI), which measures the time between jaundice and encephalopathy, is used to classify ALF, in India, the severity of encephalopathy has no bearing on survival, and ALF usually appears within 4 weeks and is caused by a relatively uniform set of factors, primarily viral hepatitis and toxins such as rodenticides.
2. Why Is Rodenticide Poisoning a Growing Cause of ALF in India?
In India, rodenticide poisoning—particularly with products containing yellow phosphorus—has emerged as a major cause of ALF, mainly in Southern areas like Tamil Nadu. A strong poison that attacks the liver, yellow phosphorus causes quick liver cell breakdown and death.
57% of 450 patients who consumed rodenticides developed ALF, and one-third of them passed away, according to the study.
Suicidal intent was the cause of the majority of rodenticide poisoning cases (97%) and was frequently brought on by social stressors.
Young adults between the ages of 15 and 34 are most impacted, indicating a concerning demographic impact.
3. How Does Rodenticide Poisoning Clinically Present and How Is It Diagnosed?

Rat Poison Causes Irreversible Liver Damage
By the time symptoms worsen, rat poison (especially yellow phosphorus) may have already caused massive hepatocellular necrosis, often needing a liver transplant. In addition to bleeding tendencies brought on by coagulopathy (impaired blood coagulation), which sometimes resembles vitamin K insufficiency, patients with rodenticide poisoning frequently exhibit indications of liver dysfunction:
Anaemia, hematuria (blood in the urine), jaundice, and disorientation (encephalopathy) are possible symptoms.
Prolonged prothrombin time (PT) and International Normalised Ratio (INR), which indicate compromised liver synthesis function and the action of vitamin K antagonists, are detected by laboratory testing.
It can be difficult to diagnose rodenticide toxicity because:
- The primary cause of clinical suspicion is inexplicable liver failure accompanied by haemorrhage.
- Sensitive tests, which are not commonly accessible, are necessary for the laboratory identification of particular rodenticide chemicals, such as the superwarfarin brodifacoum.
- If the clinical presentation raises High Suspicion of poisoning, it should not be ruled out by negative test results.
4. What Are the Main Causes of Acute Liver Failure in India Besides Rodenticide Poisoning?
Rat Poison Ingestion Often Happens in Impulsive Self-Harm. In many Indian households, rat poison is used for suicide attempts, especially among young people, due to its easy availability and lack of regulation. Although rodenticide poisoning is concerning, ALF in India is more broadly represented by:
- Hepatitis A and E viruses are the main causes of viral hepatitis (60–90%), with HEV being particularly harmful to expectant mothers.
- Drug-Induced Liver Injury (5%–15%): Ayurvedic/herbal medications and antituberculosis medications are frequent offenders.
- Other Infrequent Causes: Although uncommon, autoimmune hepatitis, Wilson’s disease, and toxic mushrooms (amanita) are significant.
A novel and developing factor, rodenticide poisoning, primarily occurs in rural and semi-urban areas.
5. What Are the Current Treatment Options and Challenges for Rodenticide-Induced ALF?


Unlike other poisons, there is no specific antidote for yellow phosphorus-based rat poison. Treatment relies on supportive care or liver transplant. Treatment of rodenticide poisoning-induced ALF is complex and resource-intensive:
- Proton pump inhibitors for gastric protection, N-acetyl cysteine (an antioxidant), vitamin K supplements if anticoagulant rodenticides are used, and gastric cleaning with activated charcoal are all part of early management.
- Monitoring: In intensive care units or high dependency units, patients need close observation of their neurological condition, coagulation profile, and liver function tests.
- Management of Cerebral Oedema: Mannitol, positioning, and cautious sedation are used to treat this potentially fatal condition.
- Although liver transplantation is still the only proven treatment, most Indian patients cannot afford it because of infrastructure constraints, organ availability, and expense. This life-saving medication is unavailable to more than 99 per cent of rodenticide ALF patients.
- By eliminating toxins and inflammatory mediators from the blood, plasma exchange, or PLEX, has become a viable treatment.. The Indian Society of Gastroenterology recommends expanding PLEX availability in district hospitals as a cost-effective strategy.
6. Why Is Prevention and Public Health Policy Crucial to Combat Rodenticide Poisoning?
Rat Poison-Induced Liver Failure Has Poor Prognosis. Without early recognition and referral to transplant centres, mortality from rat poison–induced liver failure is extremely high. Prevention is crucial because of the high death rate and limited availability of transplantation:
- limiting the availability of rodenticides that include yellow phosphorus.
- raising people’s knowledge of these toxins’ toxicity and risks.
- putting laws into place to make the use and disposal of pesticides safer.
- offering psychotherapy and mental health help to address the root causes of poisoning-related suicide attempts.
Standardised standards for diagnosis and care have been developed through collaboration between the Tamil Nadu Indian Society of Gastroenterology and the Liver Transplantation Society of India; however, widespread education and enforcement are still essential.
7. What Are the Future Directions in Research and Management?

Rat Poison Awareness Can Prevent Tragedies. Public health awareness on the lethal risks of rat poison and its mental health links can prevent its misuse and save lives. Given that rodenticide poisoning is becoming a more common cause of ALF in India,
Additional epidemiological research to monitor patterns and risk factors.
creation of quick and reasonably priced diagnostic testing.
research on supportive treatments and new antidotes outside of liver transplantation.
Expansion of regional centres’ critical care and plasma exchange infrastructure.
bolstering systems of psychosocial assistance to lower the number of suicide ingestion instances.
The management of other causes of ALF, such as paracetamol overdose, which is the main cause in Western nations, can also benefit from the techniques created for rodenticide poisoning.
Conclusion
In India, acute liver failure brought on by rodenticide poisoning is a serious and growing health issue. Due to limited access to liver transplantation, plasma exchange and the lack of particular antidotes, it disproportionately affects young adults and has a high death rate. To lessen its effects, policy-driven preventive initiatives, aggressive supportive care, early diagnosis, and awareness are crucial.
🧠 Resources to Help You Prepare, Act & Recover
-
👩⚕️ 1:1 Consultations:
Get expert guidance on liver failure and poisoning-related emergencies -
📥 Download:
Know Your Medicine (KYM) – Free eBook for liver protection & awareness -
📘 Deep Dive Guide:
Liver Transplant Made Simple – eBook & Paperback -
🧰 Recovery Resource Kit:
Complete tools, supplements & mental support for transplant healing
Seek prompt medical attention and counselling if you or anyone you know is at risk for liver illness or poisoning. We can combat this silent pandemic if we work together and implement well-informed healthcare and public health initiatives.
Frequently asked questions
What rodenticide component commonly causes hepatotoxicity in South India?
Yellow phosphorus is the main hepatotoxic agent found in many rodenticides commonly ingested, often with suicidal intent, causing severe liver damage and failure.
Why is urgent liver transplantation difficult for rodenticide poisoning patients in India?
A Tamil Nadu survey showed that over 99% of patients with rodenticide hepatotoxicity cannot access urgent liver transplantation due to limited resources and infrastructure, pushing clinicians to maximise survival using non-transplant treatments.
How does rodenticide poisoning with brodifacoum affect coagulation?
Brodifacoum is a superwarfarin that mimics vitamin K deficiency, leading to prolonged PT and PTT because it blocks vitamin K-dependent clotting factors. Treatment requires high-dose vitamin K, often for prolonged periods (sometimes months).
What is the role of Plasma Exchange (PLEX) in rodenticide-induced ALF?
The Tamil Nadu Chapter of the Indian Society of Gastroenterology recommends PLEX as an emerging, cost-effective treatment that can improve survival either alone or as a bridge to transplantation, especially where liver transplants aren’t accessible.
What clinical features characterise ALF/ acute Liver failure?
Symptoms include the sudden onset of jaundice, confusion or altered consciousness (encephalopathy), bleeding tendencies due to coagulopathy, and rapid progression over days to weeks.
How can healthcare policies address the rodenticide poisoning burden in India?
Policies could include restricting access to toxic rodenticides, promoting safe alternatives, improving emergency care infrastructure, and expanding liver transplant programs.
References
- Indian National Association for the Study of Liver (INASL) Guidelines
- Liver Transplantation Society of India (LTSI) & Tamil Nadu ISG Reports
- PubMed Articles on Acute Liver Failure and Rodenticide Poisoning
- Recent Clinical Studies from South Indian Tertiary Care Centres