The history of liver transplantation is not just a chronicle of medical milestones—it is the story of human grit, sacrifice, and unshakable vision. At the heart of this journey stands Dr. Thomas Starzl, whose nearly five decades of relentless pursuit shaped the science of transplantation and its understanding of immunology, rejection, and surgical complexity.
His contribution went far beyond operating rooms and publications; it was a life lived on the edge of possibility, where triumph was often followed by unbearable loss. In one of his final interviews, when asked if he regretted stepping away from surgery, he admitted, “I have no regrets… but I carry the pain of lives lost along the way.” That quiet confession revealed the burnout, emotional scars, and profound humanity behind the scientific revolution he led.
For those who are part of the transplant community, this history is not just about procedures and techniques—it is about the cost, the courage, and the legacy of a man who turned impossibility into reality.
Liver transplantation is one of the most remarkable achievements in modern medicine. The history of liver transplantation is a story of vision, persistence, innovation, and courage. At the centre of this journey stands Dr. Thomas Starzl, whose groundbreaking work shaped the legacy of liver transplantation and saved countless lives worldwide. This article examines the pivotal milestones in the history of liver transplantation, while also highlighting the enduring contributions of Starzl.
Pioneer in the History of Liver Transplantation
The journey of liver transplantation began with visionaries who dared to challenge the limits of medicine. Before modern techniques, liver surgery was considered highly experimental. Early pioneers faced immense scepticism, high mortality rates, and ethical dilemmas. Despite these challenges, their work laid the foundation for what would become the history of liver transplantation.
- Prolific Researcher
- Authored nearly 1,700 peer-reviewed publications, of which 461 were on liver transplantation.
- Though he pioneered kidney transplantation, his greatest legacy lies in advancing liver transplant science.
- Dog Experiments (1958–1961)
- Conducted over 150 liver transplant experiments in dogs between 1958 and 1961.
- These studies systematically addressed the multiple obstacles to successful liver transplantation.
- His meticulous experiments laid the foundation of the field at a time when the procedure seemed impossible.
- Key Contributions
- Principles of organ preservation — ensuring viability of organs outside the body.
- Transplant pathophysiology — understanding how transplanted organs interact with the recipient’s body.
- Surgical technology innovations — techniques that became applicable to all kinds of organ allografts.
- The Azathioprine Era (1962)
- Once Starzl gained access to azathioprine, a new immunosuppressive drug, he faced one last challenge: learning how to apply it effectively.
- In less than four months, through continuous liver and kidney experiments in dogs, he refined its use.
- This breakthrough transformed transplant medicine by controlling rejection and reviving hope.
- Impact on Transplant Progress
- At a time when confidence in human renal transplantation was fading, Starzl’s successes with kidneys reignited hope.
- The momentum of kidney transplantation carried liver transplantation forward, ultimately saving it from abandonment.
Challenges Before Modern Transplants
In the early 20th century, liver surgery was primarily experimental. Surgeons encountered technical difficulties, including massive bleeding, infection, and organ rejection. Many considered the idea of liver transplantation “science fiction.” These challenges shaped the early protocols and research priorities, emphasising the need for meticulous planning and innovation.
Animal studies played a crucial role in the history of liver transplantation. Researchers experimented on dogs and pigs to refine surgical techniques and immunosuppression strategies. These experiments allowed surgeons to understand vascular connections, organ preservation, and post-operative complications. The lessons learned from animal studies helped in human liver transplantation.
Early Life and Inspirations (1926–1940s)
No discussion of the history of liver transplantation is complete without Dr. Thomas Starzl. Known as the father of liver transplantation, his work represents a turning point in surgical history.
Thomas Starzl was born on March 11, 1926, in Le Mars, Iowa. His family was a fascinating mix of creativity and discipline. His father owned the local newspaper and even wrote science fiction, while his mother was a surgical nurse. You can imagine what a unique influence that must have been—words and imagination on one side, science and healing on the other.
From an early age, young Thomas was captivated by medicine. Around the age of 10 to 12, he would often watch a local physician-surgeon, Dr. Downing, as he worked. Those moments left a lasting impression and planted the seed of surgery deep within him.
Interestingly, a Navy aptitude test administered during his youth also pointed him towards a career in medicine. That small nudge, along with his own fascination, sealed his decision—he was going to dedicate his life to medical science.
In 1947, he entered Northwestern University in Chicago for medical school. After completing his studies, his journey took him to Johns Hopkins in Baltimore, where he spent about four years before moving to Jackson Memorial Hospital in Miami. Each of these places added new layers to his training, preparing him for the incredible journey ahead.
Early Career Struggles (1940s–1950s): Portal hypothesis
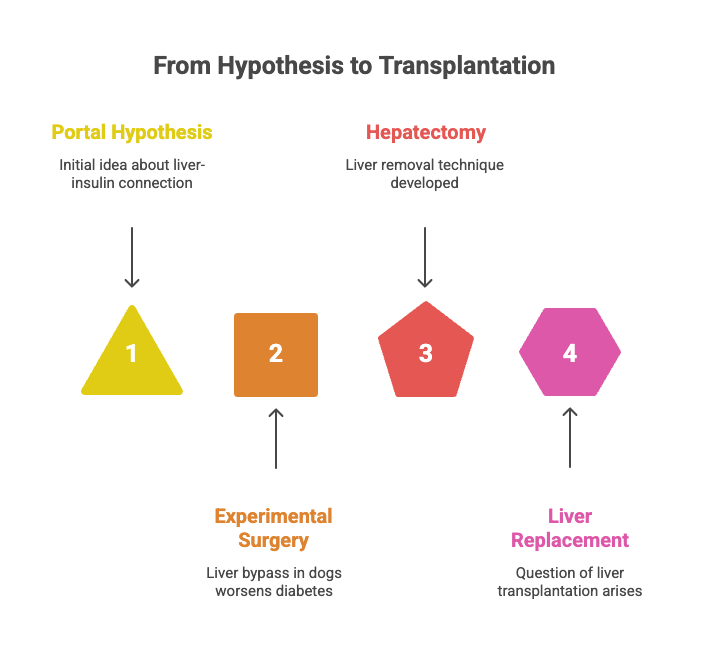
Now, let’s move into the next phase of Dr. Starzl’s journey—the 1940s and 50s—when he was laying the foundation of what would become his life’s work.
After completing medical school at Northwestern University, Thomas Starzl went on to Johns Hopkins in Baltimore, and later, to Jackson Memorial Hospital in Miami. It was here in Miami that his real struggles, experiments, and groundbreaking ideas began to take shape.
While working at the hospital, he set up his very own laboratory—not in some fancy research centre, but in a garage. That little garage became the birthplace of ideas that would transform medicine forever.
In 1955, during one of his surgeries, Starzl noticed something remarkable. After a liver bypass/ portocaval shunt, a patient’s diabetes seemed to improve. This observation lit a spark in him. He began to wonder: Could the liver, portal blood flow, and insulin be more deeply connected than anyone realised? He called this idea the Portal Hypothesis.
To test this, he turned to experimental surgery in dogs. He destroyed the pancreatic beta cells to mimic diabetes, then created a liver bypass to reroute blood. But instead of improving, the diabetes got worse. That failure was a revelation—it told him something vital was missing.
Determined to understand, he realised he had to go even further: remove the liver itself to truly see its role. That led him to develop a completely new technique for removing the liver in dogs called hepatectomy. Once he succeeded in removing the liver, he asked himself a revolutionary question: If we can take a liver out, can we also put a new one in?
At that time, he wasn’t dreaming of saving human lives yet. His only mission was to prove or disprove his portal hypothesis. But unknowingly, he had just planted the first seed of liver transplantation.
Breakthrough Experiments and Collaborations (1950s–1960s): Venovenous bypass, Double-liver fragment model, and Liver regeneration, Insulin as hepatotrophic factor
Dr. Thomas Starzl’s groundbreaking work in the 1950s and 1960s marked the critical period in which his innovative experiments and collaborations laid the foundation for modern liver transplantation.
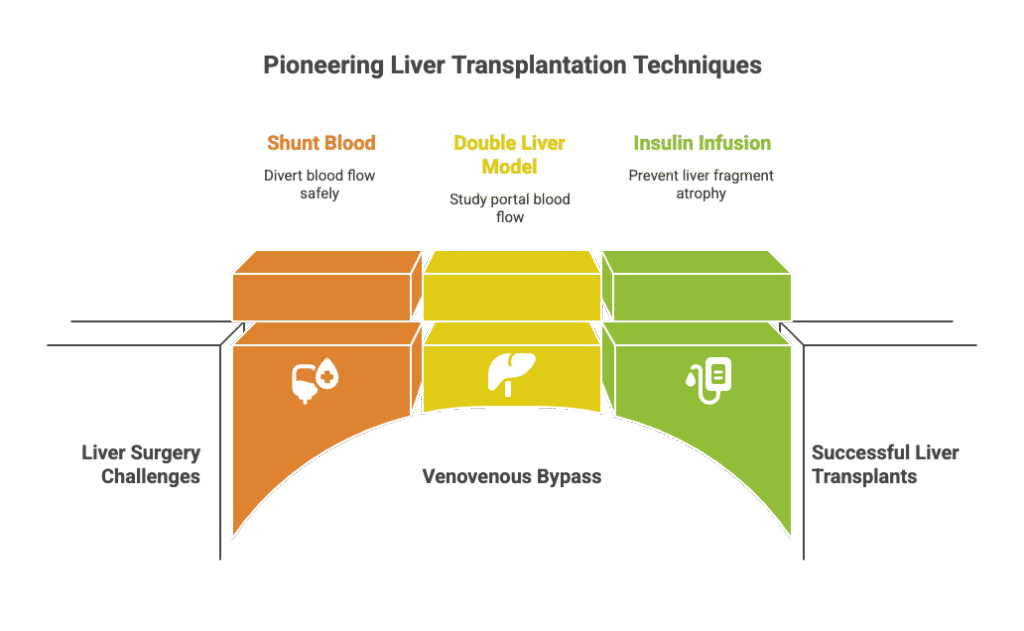
The Challenge of Portal Vein and Inferior Vena Cava Clamping
In the early stages of liver transplantation research, Dr. Starzl and his colleague, Dr. Francis Moore from Brigham, faced a significant challenge. When attempting to clamp both the portal vein and the inferior vena cava during liver surgery in animals, the dogs could not tolerate the procedure and did not survive. This obstacle hindered progress in liver transplantation techniques.
The Innovation of Venovenous Bypass
To overcome this challenge, Dr. Starzl and Dr. Moore developed the venovenous bypass technique. This innovative approach involved using plastic tubing to shunt blood from the lower body into a neck vein that drained directly into the heart. By temporarily bypassing the portal vein and inferior vena cava, this method allowed for safer and more controlled liver surgeries in animal models. This advancement marked a significant step forward in liver transplantation research.
The Double Liver Fragment Model
Building upon these surgical innovations, Dr. Starzl designed the double liver fragment model to further investigate the role of portal blood flow in liver function. In this model, the liver was divided into two fragments. One fragment received normal portal venous blood flow, while the other had its portal blood diverted via a portocaval shunt, bypassing the liver.
The results were striking. The fragment with normal portal flow remained healthy, while the fragment with diverted blood flow (portocaval shunt) rapidly atrophied. This experiment provided compelling evidence that portal venous blood contained essential factors crucial for liver health and regeneration.
Insulin Infusion and Hepatotrophic Factors
To explore the role of specific factors in liver regeneration, Dr. Starzl infused insulin into the fragment with diverted portal blood flow. Remarkably, this intervention prevented the atrophy and damage observed in the untreated fragment. This finding led to the identification of insulin as a principal hepatotrophic molecule in portal blood, essential for maintaining liver function and promoting regeneration.
Liver Regeneration Observations
Further experiments revealed that, regardless of the amount of liver tissue removed, the remaining portion consistently regenerated to its original size within three weeks. This regenerative capacity was observed to occur more rapidly in animals compared to humans. Additionally, whether the liver graft was too small or too large, it adapted to the appropriate size for the recipient, highlighting the liver’s remarkable ability to remodel itself.
“Through his pivotal experiments and collaborations, Dr. Thomas Starzl deepened our understanding of liver physiology and transplantation. He showed that portal venous blood carries vital hepatotrophic factors essential for liver survival and regeneration. These insights laid the groundwork for modern liver transplantation and continue to shape the field of hepatology.”
The Emergence of Liver Transplantation (1960s): First Human Liver Transplants, Pioneering use of Azathioprine and Steroids in Liver Transplant, Recognition of the Bleeding–Clotting Paradox and Clotting Factor use
Now let’s journey through the 1960s—a time of pioneering breakthroughs and difficult lessons in the birth of human liver transplantation.
Immunosuppression and Kidney Transplant as a Prelude
In the early 1960s, the transplant world was transformed by the arrival of pharmacological immunosuppression. Purine analogues—first 6-mercaptopurine and its derivative azathioprine—formerly experimental, began saving human kidney grafts. It’s worth remembering that, before drugs like azathioprine were available, the only way to suppress the immune system and prevent rejection was through total body irradiation.
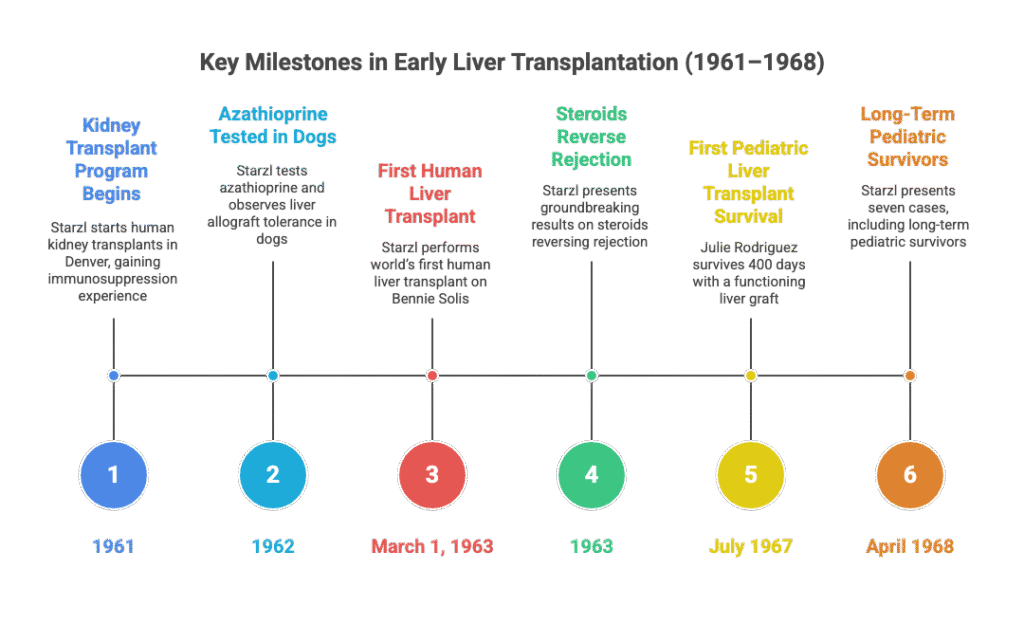
Surgeons such as David D. Hume had shown immunosuppression could prevent rejection in experimental transplants; these strategies were discussed at meetings and inspired others. Thomas Starzl, attending those gatherings, realised that to conquer liver surgery, he needed to master kidney transplantation. In 1961, upon moving to Denver as Chief of Surgery at the VA medical centre, he began performing kidney transplants in humans, combining azathioprine and steroids. These cases gave Starzl the immunosuppressive experience necessary for liver transplantation.
In 1962, Dr. Thomas Starzl made a striking observation while studying liver allografts in dogs. Even without immunosuppression, some grafts unexpectedly survived and recovered after an initial rejection phase. This hinted at the liver’s unique tolerance compared to other organs. That same year, Starzl began testing a new drug, azathioprine, on dogs. The results were promising. The true breakthrough came when he discovered that adding corticosteroids could reverse ongoing rejection episodes. This combination became the cornerstone of transplantation medicine. In 1963, Starzl presented his groundbreaking results at a National Research Council conference. He brought meticulous clinical records—detailed charts, follow-ups, and outcomes—that demonstrated consistent kidney allograft survival using his immunosuppression protocol.
The key message was revolutionary: Steroids could reverse rejection, and Azathioprine could prevent rejection.
First Human Liver Transplant – The Bennie Solis Case (March 1, 1963)
In the history of Liver Transplantation, on March 1, 1963, Starzl undertook the world’s first human liver transplant—a complex and emotionally charged surgery on a three-year-old named Bennie Solis with biliary atresia. The procedure was marred by dense adhesions from prior operations and, critically, Bennie suffered from severe clotting-factor deficiency inherent to his liver failure. At that time, cryoprecipitate or factor concentrates were not yet available (they began to enter clinical practice around 1966 following Judith Graham Pool’s discoveries in 1964).
Without the ability to restore coagulation, Bennie bled uncontrollably and tragically died during surgery. The emotional impact on the team and the family was profound. Starzl realised then that surgical mastery without effective hemostatic support was not enough—that to succeed, he would need to solve the bleeding problem too.
Pioneering Clotting-Factor Support in Transplant (Mid-1960s)
In the wake of Bennie Solis’s death, Starzl added haematology specialists to his team. As purified clotting-factor products became available mid-decade, he began administering targeted factor replacement and transfusion strategies in subsequent liver transplants. This innovation controlled intraoperative haemorrhage more effectively than before—but introduced a new problem: thrombosis.
This dual challenge—bleeding risk due to deficiency vs. clotting risk due to overtreatment—became an important lesson that wise transplantation depends on tailored coagulation management.
Persistence and Paediatric Breakthroughs (1963–1968)
Between 1963 and 1965, Starzl attempted several more liver transplants. Most failed, and a worldwide moratorium emerged across transplant centres. But he did not give up. Returning to paediatric Liver Transplant cases, on 23rd July 1967, he performed a transplant on 19-month-old Julie Rodriguez. She survived around 400 days, ultimately succumbing to metastatic disease, not graft failure. Her functioning graft marked a milestone: a working human liver transplant.
In April 1968, Starzl presented seven cases: four deaths and three survivors—Julie, plus two children named Teddy (16) and Randy (2). Later, another pediatric survivor, Kimberly, lived for more than 22 years post-transplant, establishing that liver transplantation could work—not as a hope, but as a durable reality.
Reflecting on Today
Looking back from 2025, we see that Starzl’s path was marked by technical breakthroughs, medical firsts, and profound human lessons. The advent and careful use of clotting-factor materials paved the way for managing bleeding in transplant recipients—but only when paired with tools like TEG/viscoelastic testing could we avoid tipping into a dangerous thrombotic state. Starzl’s pioneering steps in recognising and balancing those risks set the stage for the modern, measured approach we now practice.
The Evolution of Liver Transplantation: 1970s–1990s: Piggyback Liver Transplant, Triple immunosuppression(Azathioprine+ Steroid+ ATG), Cyclosporine and Steroid
Between the 1970s and 1980s, the science of transplantation began to separate from trial and error and gradually established itself as a discipline of its own. Dr Roy Calne, who had an enduring fascination with liver transplantation, played a key role in this era.
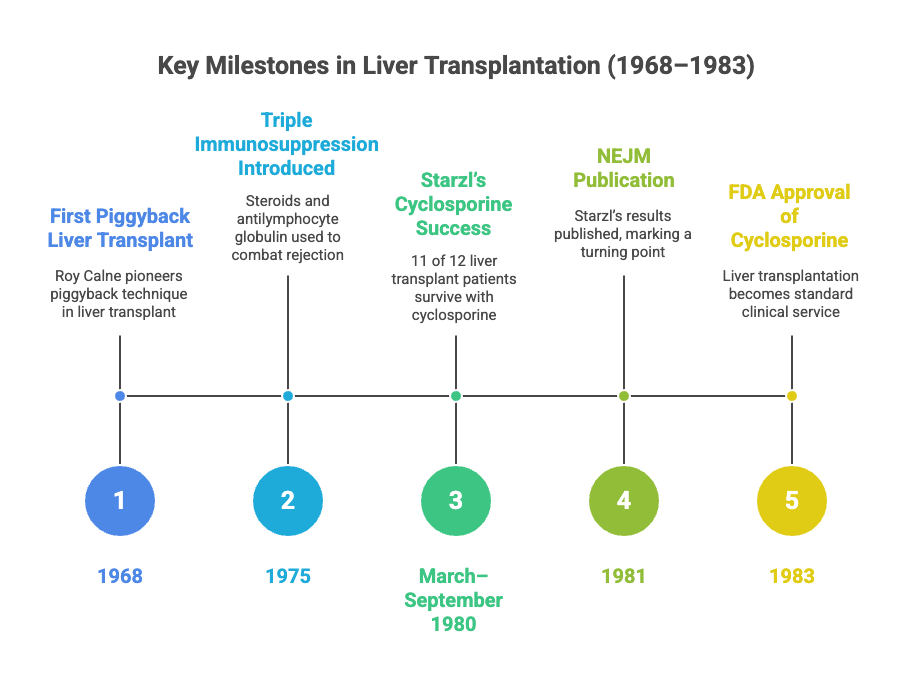
In 1968, Roy Calne performed his first liver transplant with Francis Moore. During this, he introduced the “piggyback” technique, a breakthrough in surgical innovation. The challenge arose when the donor inferior vena cava (IVC), obtained from a pediatric donor for an adult recipient, was too small. To overcome this, the donor liver was sutured to the side of the recipient’s IVC — giving birth to the piggyback method, which remains in use today.
Although the patient survived only two months due to infection, Calne persisted. He went on to perform five more such operations; tragically, four patients died. Only one — a young girl named Winnie Smith — lived for five years. During this difficult period, Calne performed the maximum number of cases worldwide, keeping the field alive despite the high mortality.
The Search for Better Immunosuppression
By 1975, a “triple immunosuppression” protocol was introduced — combining steroids with antilymphocyte globulin. Yet rejection and overwhelming infection remained major barriers, highlighting the urgent need for a new drug.
That breakthrough came with cyclosporine, introduced by Calne first in kidney transplantation and later extended to the liver. Although cyclosporine was revolutionary, its toxicity made it difficult to use widely. Around the same time, Dr. Thomas Starzl entered the scene again — and, with his relentless drive, rescued cyclosporine by modifying the protocol with added steroids. This adjustment drastically improved outcomes and brought consistency to transplantation.
The Turning Point: 1980–1983
In 1980, Starzl restarted his clinical liver transplant program. Between March and September 1980, he carried out 12 liver transplants using cyclosporine-based therapy, of which 11 patients survived. The results, published in the New England Journal of Medicine in 1981, marked a turning point in the field.
Starzl soon moved to Pittsburgh, where he performed 22 consecutive liver transplants — with all patients surviving long term. These results were unprecedented.
In 1983, the U.S. FDA approved cyclosporine, and liver transplantation was no longer considered experimental. Liver Transplantation was officially deemed a standard clinical service. Within a year, nearly 600 liver transplants were performed globally, many under Starzl’s direct training programs.
Advances and New Horizons: Tacrolimus, Microchimerism and Immune Tolerance
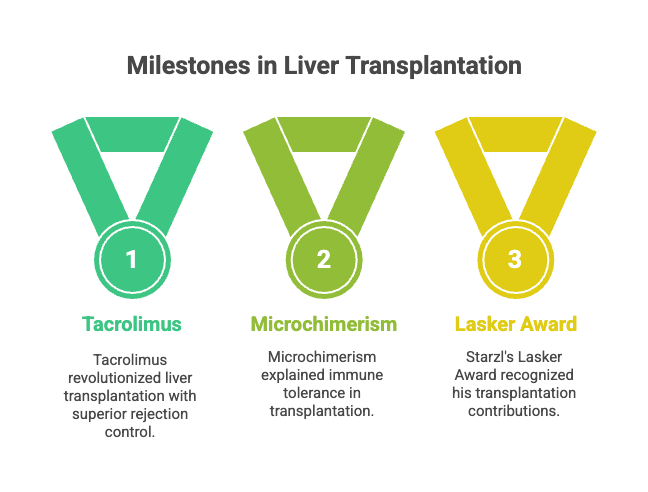
By the late 1980s, another major immunosuppressant, tacrolimus (FK-506), entered clinical use. Introduced in 1989, it offered even better control of rejection, further cementing transplantation as a dependable therapy.
Starzl’s vision went beyond survival. He highlighted that liver transplantation could also treat inherited metabolic disorders, paving the way for cures beyond end-stage liver failure. In 1992, he introduced the concept of microchimerism, describing how donor leukocytes migrate into the recipient and induce a state of immune tolerance — a discovery that shaped modern transplant immunology.
Over the next 25 years, Starzl remained deeply committed to research and mentorship. His work earned him the Lasker Award in 2012, one of medicine’s highest honours. He often reflected that what had begun as a “dream and fantasy” had, by the time of his lifetime, become an accepted, life-saving service.
A Legacy of Courage and Persistence
Dr. Thomas Starzl passed away on March 4, 2017, just a week before his 91st birthday. His life’s work reminds us that medicine is not merely about science and protocols but about courage, persistence, and the unwavering spirit to save lives.
Through his relentless pursuit, the science of liver transplantation transformed from impossible experimentation into a global clinical service — giving hope and survival to patients who once had none.
Patchwork Philosophy and Human Impact
Starzl described liver transplantation as a “whimsical, imaginative work involving patchwork,” highlighting that success comes from incremental solutions to complex problems.
His work has transformed thousands of lives, embodying compassion, resilience, and human ingenuity.
Conclusion: The History of Liver Transplantation and Starzl’s Legacy
The history of liver transplantation is inseparable from the legacy of Dr. Thomas Starzl. From early tragedies to groundbreaking successes, Starzl’s vision, persistence, and innovation transformed liver transplantation into a life-saving medical procedure. His teachings, research, and mentorship continue to guide surgeons worldwide, ensuring that the dream of liver transplantation remains a reality for future generations.
Dr Starzl’s journey exemplifies how perseverance, innovation, and human compassion can rewrite the course of medical history. The history of liver transplantation is ultimately a story of hope, courage, and the enduring legacy of Dr Thomas Starzl.
Frequently Asked Questions: History of Liver Transplantation & Legacy of Dr Thomas Starzl
What is the history of liver transplantation?
The history of liver transplantation began in the 1960s with pioneering surgeons experimenting on animals and performing the first human liver transplants. Early surgeries faced high mortality rates, but continuous innovations in surgery, immunosuppression, and post-operative care gradually transformed liver transplantation into a standard medical procedure.
Who is Dr. Thomas Starzl, and why is he important in liver transplantation?
Dr Thomas Starzl is widely regarded as the father of modern liver transplantation. His groundbreaking surgeries, research in immunosuppression, and global mentorship established the legacy of Dr. Thomas Starzl and shaped the modern practice of liver transplantation.
What were the first liver transplant surgeries performed by Dr. Thomas Starzl?
Starzl’s first pediatric transplant was performed on Beni Solis in 1963, which ended tragically due to bleeding complications. He later performed surgeries on children like Judy Roderick and Kimberly, who demonstrated the potential for long-term survival, forming critical milestones in the history of liver transplantation.
How did Dr. Starzl contribute to immunosuppression in liver transplants?
Dr Starzl introduced the use of drugs like azathioprine, steroids, and later cyclosporine and Tacrolimus in Liver Transplantation. These innovations drastically improved transplant survival rates and helped establish liver transplantation as a standard treatment.
What is the significance of the piggyback liver transplant in history?
The first piggyback liver transplant, performed by Dr. Roy Calne in England, preserved the recipient’s inferior vena cava. This innovation, along with Starzl’s techniques, contributed to the evolving surgical protocols and is a key milestone in the history of liver transplantation.
How did liver transplantation evolve from experimental to standard care?
Through decades of research, clinical trials, and innovations in immunosuppression, liver transplantation moved from high-risk experimental surgery to an FDA-approved, insured procedure by 1983. Starzl’s work played a central role in this transformation.
What is the global legacy of Dr. Thomas Starzl?
Beyond his surgeries, Starzl trained hundreds of fellows worldwide, spreading liver transplantation expertise. His legacy includes surgical techniques, immunology research, and a framework for global liver transplant programs.
What are some key milestones in the history of liver transplantation?
- Early animal experiments and hepatectomy techniques
- First human pediatric liver transplant (Bennie Solis, 1963)
- Successful long-term paediatric survival (Kimberly)
- Introduction of immunosuppression therapy (1970s)
- FDA approval of cyclosporine (1983)
Why is liver transplantation considered a life-saving procedure today?
Thanks to the history of liver transplantation and innovations by Dr. Starzl and other pioneers, liver transplantation now offers long-term survival and improved quality of life for patients with end-stage liver disease, biliary atresia, and liver cancer.
How can someone learn more about the legacy of Dr. Thomas Starzl?
The legacy of Dr. Thomas Starzl is documented in medical journals, biographies, and transplant history books. Visiting major liver transplant centres and reviewing research publications by Starzl provides insight into his contributions and the evolution of liver transplantation.