Liver cancer, especially hepatocellular carcinoma (HCC), is the sixth most commonly diagnosed cancer and the third leading cause of cancer-related death globally.
Chronic liver disease, cirrhosis, hepatitis B/C, and alcohol abuse are common risk factors.
For eligible patients, liver transplantation not only removes the cancer but also cures the underlying liver dysfunction, offering a double benefit. This article explores why liver transplant is a powerful option for treating liver cancer, with updated guidelines and recent research from AASLD, EASL, Liver Transplantation and PubMed.
Understanding Liver Cancer Types and Treatment
Types of Liver Cancer
- Hepatocellular Carcinoma (HCC): Most common, often linked to cirrhosis or hepatitis.
- Cholangiocarcinoma: Cancer of the bile ducts inside the liver; harder to treat.
- Hepatoblastoma: Rare, mostly in children.
- Secondary Liver Cancer (Metastatic): Cancer from other organs that spreads to the liver.
✅ Add-On: Brief Explanation
Hepatocellular Carcinoma (HCC): Most common primary liver cancer; usually arises in cirrhosis.
Cholangiocarcinoma: Cancer of bile ducts inside or near the liver; limited transplant eligibility; high recurrence.
Hepatoblastoma: Rare childhood liver cancer; surgery + chemotherapy often curative.
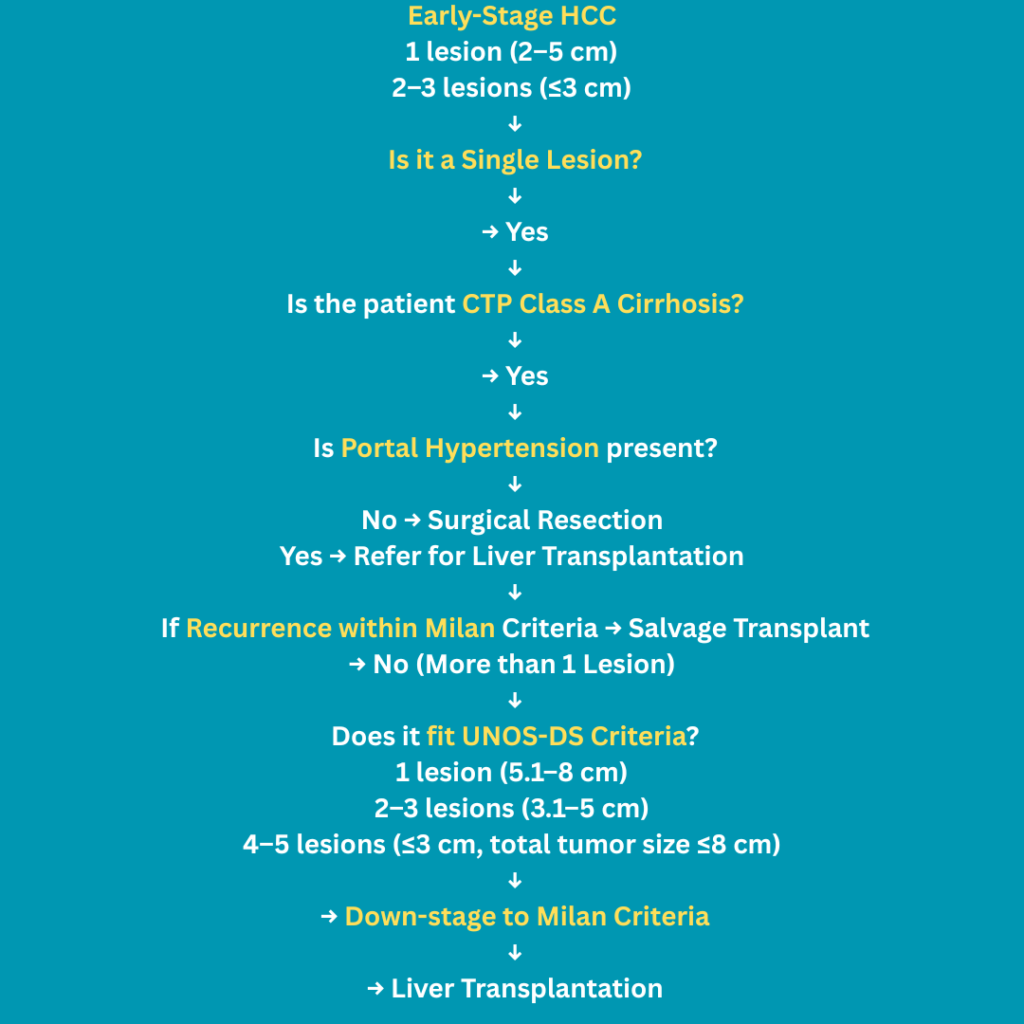
Secondary Liver Cancer: Metastasis from other cancers (colon, breast, pancreas); transplant not indicated.🟢 HCC Treatment Algorithm (Based on Child Score, Tumour Size & Number)
Hepatocellular carcinoma (HCC) treatment depends on liver function (Child-Pugh score), portal hypertension, number and size of tumours, and whether the cancer has spread. While some treatments aim to cure, others help control symptoms or slow the cancer’s growth. Here’s a simplified overview:
📝 Notes for Better Understanding:
- Child A: Indicates preserved liver function. More treatment options (RFA, Resection).
- Child B/C: Decompensated liver. Often, only transplant or palliative care is feasible.
- Milan Criteria: Single tumour ≤5 cm or up to 3 tumours ≤3 Cm each.
- Portal Hypertension: Limits surgical options to Liver Transplant only.
- RFA (Radiofrequency Ablation): Minimally invasive, curative in single small tumours.
- TACE / TARE: Used when transplant is not feasible, to downstage tumours.
- Sorafenib / Lenvatinib: Oral drugs used in advanced stages.
"Cure is possible when cancer and liver work together. When they don't, control is still a victory."Symptoms and Disease Progression

- Early Symptoms: Fatigue, right upper abdominal pain, weight loss, loss of appetite.
- Advanced Symptoms: Jaundice, ascites (fluid in abdomen), confusion, bleeding tendency.
- Progression: As tumours grow, they invade blood vessels, spread to lymph nodes/lungs, or rupture, leading to emergencies.
"The body whispers before it screams. Early diagnosis saves lives."1. Liver Cancer Operability
Surgical resection is often not possible in liver cancer due to cirrhosis or tumor location. Liver transplantation replaces the entire liver, removing both the tumour and the diseased liver tissue. According to AASLD guidelines, patients with early-stage HCC who meet transplant criteria have excellent outcomes.
"Where there is life, there is hope."2. Liver Transplant Criteria For Liver Cancer

Milan Criteria
One tumor ≤5 cm, or
Up to three tumors, each ≤3 cm
No vascular invasion or extrahepatic spreadExpanded Criteria (e.g., UCSF)
One tumor ≤6.5 cm or up to 3 tumors with total diameter ≤10 cmRecent studies show patients outside the Milan Criteria but within UCSF Criteria have comparable outcomes. Downstaging therapies like TACE can help patients become eligible for Liver Transplant.
"Eligibility isn’t a door; it’s a path."3. Liver Cancer: Better Outcomes After Liver Transplant
Patients within Milan or UCSF criteria who undergo transplantation have:
- 5-year survival rates >70%
- Lower recurrence rates
Compared to resection, transplant addresses both the tumour and cirrhotic liver, minimising recurrence. Latest data confirms survival advantage, especially in cirrhotic patients.
"Healing doesn’t mean the damage never existed. It means the damage no longer controls our lives."
4. Living Donor Liver Transplant Speeds Up Treatment
Due to the deceased donor shortage, Living Donor Liver Transplant (LDLT) is gaining traction in Asia and India.
LDLT Adds to Success Rate in Liver Cancer: Here’s Why
Living Donor Liver Transplantation (LDLT) has revolutionised liver cancer care, especially in regions with long waiting times for deceased donor organs. It’s not just a time-saving alternative—it significantly improves survival and treatment outcomes when used in carefully selected liver cancer patients, particularly those with Hepatocellular Carcinoma (HCC).
✅ Timely Surgery Improves Outcomes
Waiting for a deceased donor liver can take months, during which liver cancer may grow beyond transplant criteria (Milan or UCSF), disqualifying the patient.
LDLT avoids this risk by allowing scheduled surgery at an optimal time, reducing waitlist dropout.“The clock is the enemy in cancer care. LDLT helps beat it.”
✅ LDLT Enables Transplant in Early Stages
Patients with early-stage HCC and stable liver function are ideal candidates.
By transplanting before the tumour spreads or liver decompensation, LDLT leads to better overall survival and fewer complications.
✅ LDLT Equal or Better Survival than DDLT
Studies confirm that LDLT has:
- 5-year survival rates >70–80%
- Similar or lower recurrence rates compared to Deceased Donor Liver Transplant (DDLT)
- Better preoperative planning and optimisation
“Success isn’t just survival—it’s quality, timing, and a full life ahead.”
✅ Expands Access in Resource-Limited Settings
In countries like India, where deceased organ donation is limited,
LDLT:
- Makes transplant more accessible and affordable
- Encourages family involvement and awareness
- It is offered by many high-volume centres with excellent outcomes
✅ Safer Than Ever Before
Modern surgical techniques have dramatically reduced the risk to the donor.
Living donors undergo:
- Extensive evaluation
- Minimally invasive surgery in many cases
- Quick recovery with low complication rates
“A living donor doesn’t just give part of their liver—they give a second chance at life.
5. How Surgical Approach Depends on Tumour and Liver Health
The choice between liver resection, transplantation, or other therapies is not one-size-fits-all. It depends on two key factors:
🧠 1. Tumor Burden – size, number, and location of tumors
🫀 2. Liver Function – how well the liver is working (Child-Pugh score, MELD score, presence of cirrhosis)✅ Liver Resection (Surgical Removal)
Best for patients with good liver function (no or early cirrhosis) and localized tumors.
Offers long-term survival when cancer is fully removed and liver reserve is strong.
Often done in non-cirrhotic HCC or intrahepatic cholangiocarcinoma.🟢 Ideal for:
– Single tumor
– No portal hypertension
– Child-Pugh A liver
– Low MELD score
“When the liver is strong, cutting out cancer gives a real shot at cure.”
✅ Liver Transplantation
Preferred when the patient has advanced cirrhosis or poor liver function.
Also ideal if the tumor fits within Milan or UCSF criteria (limited size and number).
Transplant treats both cancer and cirrhosis, offering the best chance of long-term survival.
Living donor liver transplant (LDLT) offers flexibility and early access.🟢 Ideal for:
– HCC within transplant criteria
– Decompensated cirrhosis
– High MELD scores
– Tumors not suitable for resection“A new liver can mean a new life—free from both cancer and cirrhosis.”
✅ Bridging Therapies (While Waiting for Transplant or to Downstage Tumour)
Sometimes, patients are not immediately eligible for surgery or a transplant. In such cases, bridging therapies are used to control or shrink the tumour:
TACE (Transarterial Chemoembolization)
Blocks tumor blood supply and delivers chemotherapy directly to the tumor.
RFA (Radiofrequency Ablation)
Burns small tumors using heat through a special needle.
SBRT (Stereotactic Body Radiation Therapy)
Delivers highly focused radiation to tumors with minimal damage to normal liver.TACE/ RFA/ SBRT:
Prevent tumor progression while waiting for a transplant
Downstage tumors to make patients eligible for surgery/transplant
Are especially useful in DDLT waitlist scenarios to avoid dropout“When timing is crucial, bridging therapies buy hope, and time.”
⚖️ The Decision Is Individualised
There is no single best option for everyone. The surgical approach depends on:
Tumor characteristics (size, number, spread)
Liver reserve and presence of cirrhosis
Comorbidities (heart, kidney issues)
Patient age, fitness, and preferences
Donor availability and urgencyThat’s why Multidisciplinary Team (MDT) discussions are vital. Surgeons, hepatologists, radiologists, and transplant specialists come together to create a personalised plan that offers the best chance of success.
“Your treatment isn’t chosen from a menu. It’s crafted just for you.”
6. Liver Cancer Prognosis Depends on More Than Stage
🧭 Key Factors That Influence Liver Cancer Prognosis
Every liver cancer story is different. Some patients respond well to treatment and thrive for years, while others may face aggressive disease. Understanding the factors that influence prognosis helps patients and caregivers make informed decisions and set realistic expectations.
Let’s break them down:
🟠 Tumour Size and Number
Smaller tumors (usually <5 cm) and fewer nodules have a better prognosis.
Single tumors often qualify for resection or transplant.
Multiple large tumors are harder to treat and may indicate spread.📌 Supported by: Multiple studies, including the Milan and UCSF criteria, which use size/number to determine transplant eligibility and survival prediction.
“In liver cancer, less is often more—fewer and smaller tumors give more options.”
🟠 AFP Levels (Alpha-Fetoprotein)
AFP is a tumor marker—a blood test that may reflect tumor activity.
High AFP (>400–500 ng/mL) is associated with:
- Advanced disease
- Poorer differentiation
- Higher recurrence post-transplant“AFP is not just a number—it’s a whisper from the tumor.”
🟠 Histologic Grade Tumour Cell Type)
Tumors may be well, moderately, or poorly differentiated.
Poorly differentiated tumors grow faster, spread more, and have a worse outcome.
Grading is only confirmed after biopsy or surgery, but imaging clues may help.📌 Clinical Insight: Histology is now being integrated into AI-based prediction models for better staging.
🧠 Role of AI:
“AI is transforming liver cancer care—analyzing scans, labs, and tumor patterns to predict prognosis and personalize treatment like never before.”“The nature of cancer cells tells us how fierce the fight will be.”
🟠 Liver Reserve (MELD & Child-Pugh Scores)
A strong liver can withstand major surgery or transplant; a failing liver cannot.
Child-Pugh score assesses cirrhosis severity (A to C).
MELD score (Model for End-stage Liver Disease) helps prioritize for transplant.📌 Recent Findings:
Child-Pugh A patients undergoing resection had better survival than Child B/C patients on non-curative therapy.
“Cancer is one enemy, but liver failure is another. Both must be tackled together.”
🟠 Response to Bridging or Downstaging Therapies
- If a tumour responds well to TACE, RFA, or SBRT, the outcome post-transplant or surgery improves.
- A good response often indicates biologically favourable tumours.
- Poor response may signal aggressive disease.
📌 Insight:
An analysis showed that patients who had complete or partial tumour necrosis on bridging therapy had 40–60% lower recurrence rates post-transplant.
“When cancer retreats under fire, it often means we’re winning.”
🧪 Prognosis Is a Puzzle — Not a Prediction
Each of these factors plays a role, but no single factor tells the full story. Doctors look at the complete picture
—your liver function, tumor biology, blood markers, and how the disease behaves over time—to tailor your care.🎯 The goal is not just to treat, but to give time, quality, and hope.
“Your prognosis is not set in stone—it’s shaped every day by decisions, responses, and resilience.”
7. Latest Advances in Liver Cancer & Transplant
2024 hepatocellular carcinoma (HCC) guidelines by EASL, AASLD, and APASL—introduce several significant updates, which include surveillance every 6 months to rule out recurrence
Surveillance
Ultrasound + AFP every 6 months; CT/MRI for high-risk cases.🩸 Machine Perfusion: Revolutionising Organ Preservation
Traditionally, donor livers are preserved on ice (static cold storage), which limits how long and how well they stay viable. Machine perfusion is a breakthrough technology that pumps oxygenated blood or preservation fluid through the donor liver at controlled temperatures—either cold (hypothermic) or body temperature (normothermic). This technique:
Reduces graft rejection and complications
Extends the safe preservation time of donor livers
It’s already being used in top transplant centers globally and holds promise for expanding the donor pool and improving transplant outcomes.🧬 Adjuvant Immunotherapy Post-Curative Treatment
The NCCN 2024 guidelines recommend considering adjuvant therapy with atezolizumab plus bevacizumab for patients at high risk of recurrence after resection or ablation. High-risk features include:
- Tumor size >5 cm
- More than 3 tumours
- Macrovascular or microvascular invasion
- Grade 3/4 histology
This recommendation is based on interim results from a Phase III trial showing improved recurrence-free survival at 12 months, though overall survival benefits are yet to be established.
🧪 Combining Immunotherapy and Transplant (Emerging Strategy):
Recent clinical trials and case studies are exploring whether immunotherapy—typically used for advanced HCC—can be safely combined with liver transplantation after a carefully timed washout period (usually several weeks to months).
This break allows the immune system to reset and reduces the risk of graft rejection. While not yet standard practice, this evolving strategy holds promise for selected patients with initially inoperable or borderline tumours.
“The future is not a place we go; it’s a place we create.”
🟢 Conclusion: A New Dawn for Liver Cancer Patients

Liver transplant continues to stand as a gold standard and potentially life-saving treatment for select liver cancer patients, especially those with hepatocellular carcinoma within established criteria. It not only removes the tumour but also replaces the diseased liver, offering a dual cure.
Success depends on several key factors: early diagnosis, strict eligibility assessment, timely surgical planning, and vigilant post-transplant care. The integration of living donor liver transplants (LDLT) has dramatically improved access and outcomes, especially in regions where deceased donor organs are scarce.
With exciting innovations like machine perfusion, AI-guided imaging, and research into combining immunotherapy with transplantation, the future of liver cancer treatment is brighter than ever. These advancements are not just extending lives—they’re restoring quality of life.
Let this message offer hope:
A liver cancer diagnosis doesn’t have to be the end of the road. For many, it can be the beginning of a second chance.🌿 Book a Online Consultation with Dr. Tanuja Mallik
For personalised guidance, you can book a one-on-one consultation using the secure payment link below:
👉 Click here to make your payment
Once your payment is confirmed, please choose your convenient time for the consultation:
📅 Schedule your appointment via Calendly
After booking, we can connect via WhatsApp or Zoom — whichever is more comfortable for you.
💬 Have questions before you book? Feel free to reach out! I’m here to help.
Warm regards,
Dr. Tanuja Mallik
Frequently Asked Questions
How long can you live with liver cancer?
Survival depends on the stage, overall health, and treatment options. With early diagnosis and treatment (including transplant), many patients live for years. Late-stage cancer may shorten life expectancy, but supportive care can still improve quality of life.
Is cancer of the liver curable?
Yes, if detected early. Surgery, ablation, or a liver transplant can offer a potential cure. In advanced stages, treatments may not cure but can prolong life and ease symptoms.
What are the first signs of liver cancer?
Often silent in early stages. When symptoms appear, they may include fatigue, unexplained weight loss, right upper abdominal pain, jaundice (yellowing of eyes/skin), or abdominal swelling.
Can stage 4 liver cancer be cured?
Cure is rare at this stage, but treatments like immunotherapy, targeted therapy, or palliative care can help manage symptoms and potentially extend life.
What causes liver cancer?
Major causes include chronic hepatitis B or C, alcoholic liver disease, non-alcoholic fatty liver disease (NAFLD), cirrhosis, and certain toxins or genetic disorders.
What are the symptoms of liver cancer?
- Persistent abdominal discomfort
- Sudden weight loss
- Loss of appetite
- Fatigue and weakness
- Nausea or vomiting
- Swollen abdomen or legs
- Jaundice
Can liver cancer lead to a liver transplant?
Yes. In selected patients with early-stage liver cancer, a liver transplant is not just possible—it’s one of the most effective curative options.
About the Author
Dr. Tanuja Mallik is a liver transplant anaesthetist and critical care specialist with years of experience in managing complex transplant cases.Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider for personalized guidance.

A well directed and meaningful discourse offering a broad and educative data to the patients keen to know more about their disease.
Thank you so much Dr Puneet 🙂 I hope it helps the patient and their caregiver.