Podcast in English
Podcast in Hindi
Liver transplant rejection is a critical concern after liver transplantation (LT), where the recipient’s immune system may recognise the new liver as foreign and attempt to attack it. If not detected and treated early, rejection can lead to irreversible liver damage or graft loss.
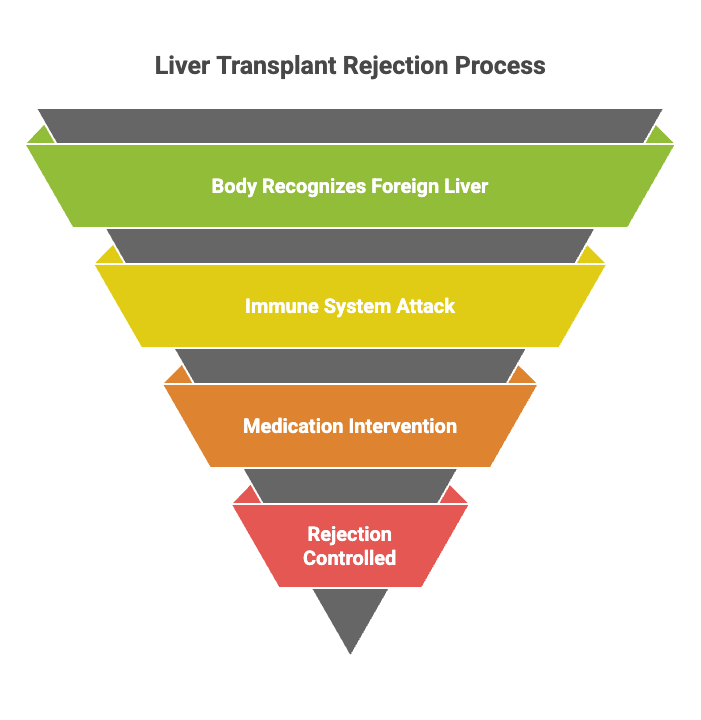
Analogy for patients: Think of your body as a security system. When a new liver is transplanted, the system may mistakenly identify it as an intruder. Medications act like security guards, calming the system and protecting the liver.
This blog explains rejection in simple terms for patients and families while also providing detailed immunology insights for healthcare professionals.
Starzl’s Microchimerism Paradigm
- Core Concept
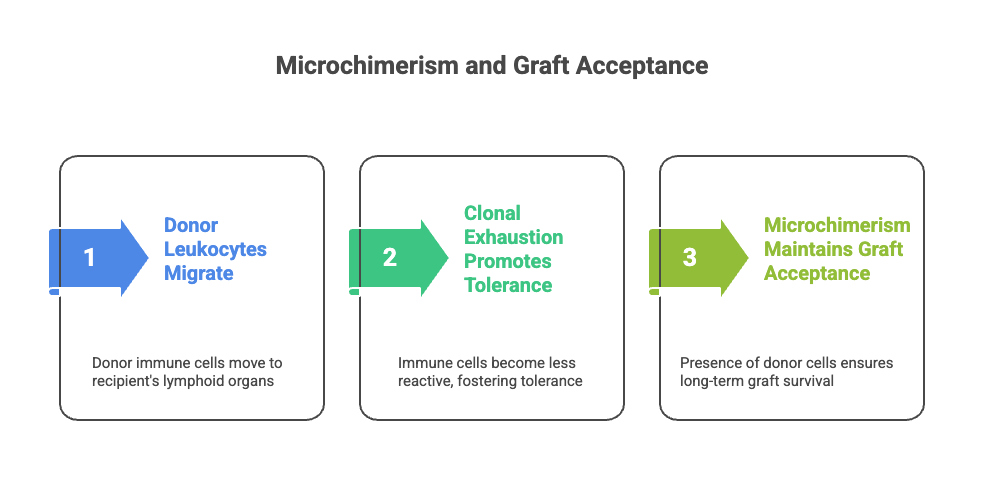
- After liver transplantation, donor leukocytes migrate into the recipient’s lymphoid organs.
- This migration results in a two-way immune conversation: donor and recipient cells recognise each other, initially clash, and then gradually undergo clonal exhaustion and peripheral deletion.
- The outcome is microchimerism—a stable, low-level coexistence of donor leukocytes within the recipient. Microchimerism refers to the persistence of a small number of donor-derived cells (<1% of total circulating cells) in the recipient after transplantation.
- These donor cells are multilineage and migrate to various recipient tissues, where they interact with the host immune system.
- Microchimerism is strongly associated with long-term graft tolerance and a reduced incidence of rejection episodes.
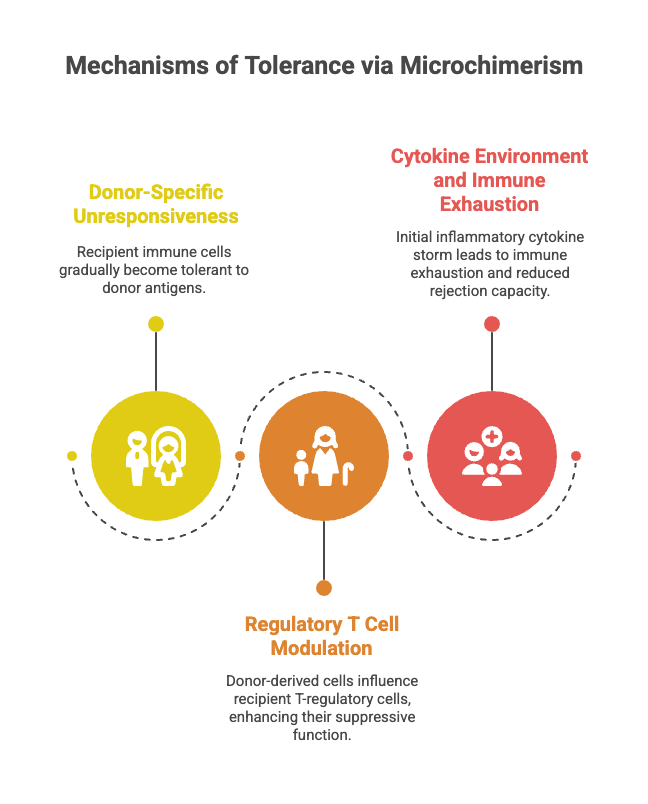
- Mechanisms of Tolerance via Microchimerism
1. Donor-Specific Unresponsiveness
Recipient immune cells gradually become tolerant to donor antigens.
Analogy: Like a bridegroom who initially resists a new bride’s habits but, over time, accepts her ways as part of daily life.
2. Regulatory T Cell Modulation
Donor-derived cells influence recipient T regulatory cells (Tregs), thereby enhancing their suppressive function.
This reduces immune activation against the graft.
Analogy: Think of the mother-in-law (Tregs) who regulates the household. The bride (donor cells) gradually wins her over, leading to household harmony and suppression of family conflicts.
3. Cytokine Environment and Immune Exhaustion
Initially, transplantation triggers an inflammatory cytokine storm, much like family resistance to a newcomer.
Over time, repeated activation leads to immune exhaustion, with diminishing capacity for rejection.
Analogy: The extended family keeps criticising the bride at first, but eventually, they tire of complaining and adapt, leading to peace.
Starzl’s Key Observations
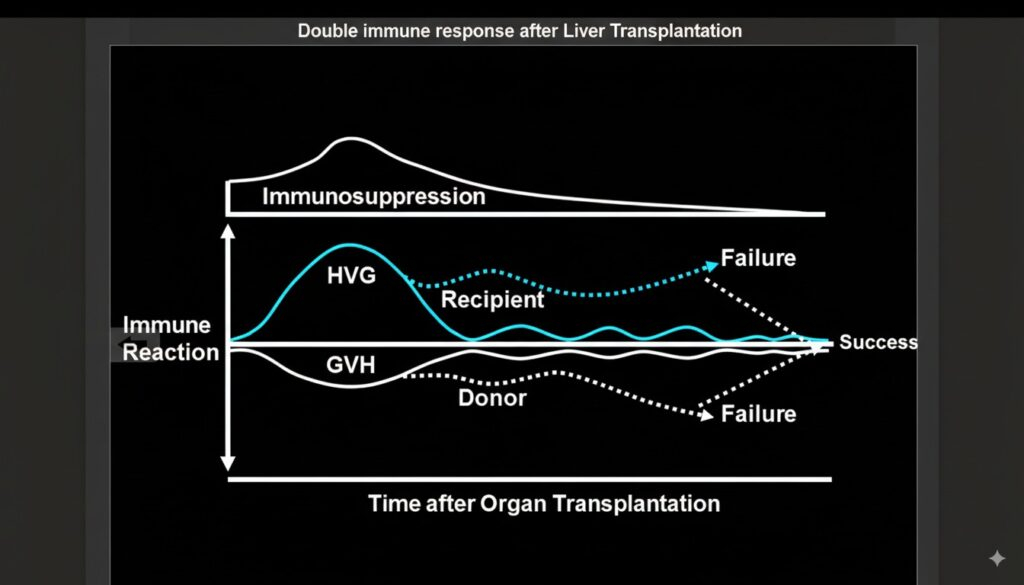
- Rejection ≠ Failure, but a Turning Point
- Cell migration and microchimerism occur after organ transplantation, followed by graft acceptance.
- Starzl suggested that the onset of rejection often coincides with its reversal and the beginning of variable immune tolerance ( double immune response).
- When treated with “steroid boluses”, rejection could often be reversed.
- After reversal, the overall requirement for immunosuppression declines, since the immune system is already learning tolerance.
- Cell migration and microchimerism occur after organ transplantation, followed by graft acceptance.
- Immunosuppression Strategy
- Pre-transplant immunosuppression (if feasible) → prepares the host for tolerance.
- Post-transplant → aim for monotherapy (single agent, usually a CNI).
- Steroids should be reserved for rejection crises, not lifelong use.
- High-dose or continuous immunosuppression may be harmful, as it risks destroying donor leukocytes that are essential for tolerance.
- Passenger Leukocytes
- Around 20% of organ mass consists of donor-derived leukocytes (bone marrow origin).
- Their migration is like giving a mini bone marrow infusion, critical for tolerance induction.
- Over time, most disappear, leaving behind self-renewing microchimeric donor cells that help maintain acceptance.
- Experimental Findings
- In animal models (dogs, baboons, chimpanzees), xenotransplants failed not due to T-cell rejection but because of complement activation, which cannot be controlled by tacrolimus or azathioprine.
- This explained survival windows of 26–70 days in xenograft experiments.
Bride–Bridegroom Analogy for Microchimerism

- The Wedding (Transplant Event)
- The bride (donor organ & leukocytes) joins the groom’s family (recipient immune system).
- At first, both sides resist: the family doubts the bride, and the bride struggles with the family’s ways.
- Early Conflicts (Rejection)
- Arguments break out, symbolising immune attacks.
- But during this very conflict, both sides begin to understand that they cannot constantly fight.
- Exhaustion and Tolerance
- Over time, both bride and family grow tired of the battles (clonal exhaustion).
- They start accepting each other’s differences and reach a working harmony (peripheral deletion + tolerance).
- The Role of Steroids (Mediator)
- When conflicts peak, a “mediator” (pulse steroids) may step in to calm things down.
- Once peace is restored, the mediator withdraws, and the family continues in relative harmony without constant outside interference.
- The Balance of Presence
- The bride must stay present in the family (donor leukocytes must persist).
- If she disappears completely (donor cells lost), the family dominates, and the marriage collapses—symbolising graft rejection.
Starzl’s Practical Message
- Do not aim to kill donor leukocytes completely → they are the foundation of tolerance.
- Do not rely on lifelong heavy immunosuppression → it causes toxicity without aiding long-term acceptance.
- Rejection is not the end → it often marks the beginning of tolerance.
- Operational tolerance is possible → in some patients, long-term survival with minimal or no immunosuppression is achievable.
👉 So, in essence, “microchimerism is like a marriage”
- Initial clashes are normal (early rejection).
- Patience and mediation (pulse steroids) can restore peace.
- Long-term coexistence (microchimerism) creates a stable family life (graft survival), but only if both sides remain present and tolerant.
Patient-Friendly Core Sections on Liver Transplant Rejection
1. What is Liver Transplant Rejection?
Rejection occurs when the recipient’s immune system recognises donor liver cells as foreign and mounts an attack. This immune response can happen early (within weeks or months) or late (years after transplant).
Patient analogy: Imagine planting a new tree in your garden. Sometimes, nearby plants (the immune system) may grow over it and block its sunlight, stunting its growth. Medicines work like gardeners, giving the new tree space to thrive.
Most rejections are treatable if detected early. Rejection does not mean failure—it is a signal to adjust medications and care.
2. Types of Liver Transplant Rejection Every Patient Should Know
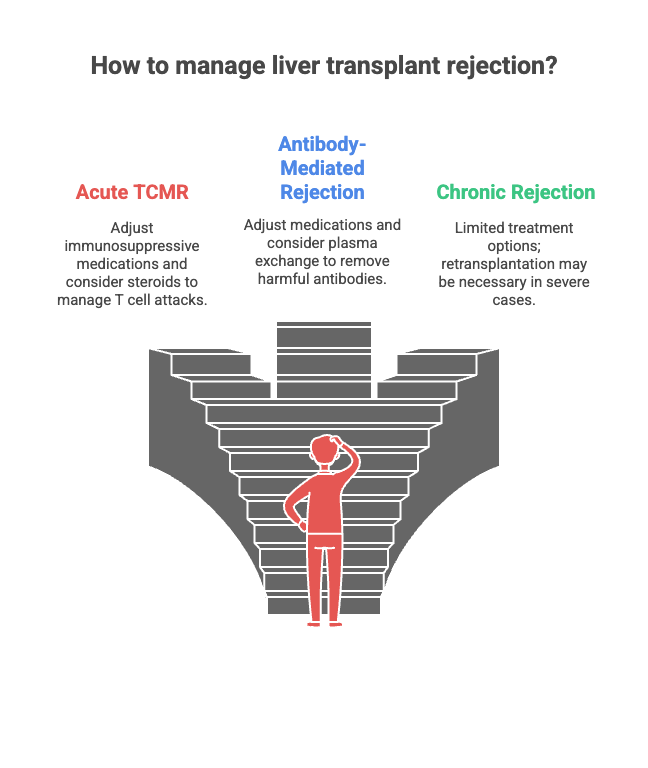
Liver transplant rejection is classified into three main types:
- Acute T Cell-Mediated Rejection (TCMR)
- Timing: Typically occurs within the first 3 months.
- Mechanism: The recipient’s T cells identify donor antigens (MHC molecules) and attack liver cells.
- Treatment: Adjusting immunosuppressive medications; steroids may be added if needed.
- Patient analogy: Think of T cells as soldiers. Sometimes they mistake the new liver for an enemy. Medicines act like peacekeepers, telling the soldiers to stand down.
- Antibody-Mediated Rejection (AMR)
- Timing: Can occur at any time after transplant, although it is rare (<1%).
- Mechanism: Donor-specific antibodies (DSAs) bind to liver cells, triggering the complement system, causing inflammation and cell damage.
- Treatment: Medication adjustment, sometimes plasma exchange to remove harmful antibodies.
- Patient analogy: Antibodies are like missiles targeting the liver. Doctors can redirect or remove the missiles before they cause damage.
- Chronic Rejection
- Timing: Months to years after transplant.
- Mechanism: Progressive injury leads to bile duct loss and fibrosis. Often results from repeated acute rejection episodes or a single severe AMR.
- Treatment: Limited; retransplantation may be required in severe cases.
- Patient analogy: Chronic rejection is like slow rusting of metal—preventive maintenance (early treatment) is essential to stop damage.
| Type | Timing | Mechanism | Treatment |
| TCMR | 1–3 months | Med adjustment, steroids | Meds adjustment, steroids |
| AMR | Anytime | Donor-specific antibodies + complement | Meds, plasma exchange |
| Chronic | Months–years | Progressive fibrosis, bile duct loss | Often irreversible, retransplant |
3. Warning Signs of Liver Transplant Rejection
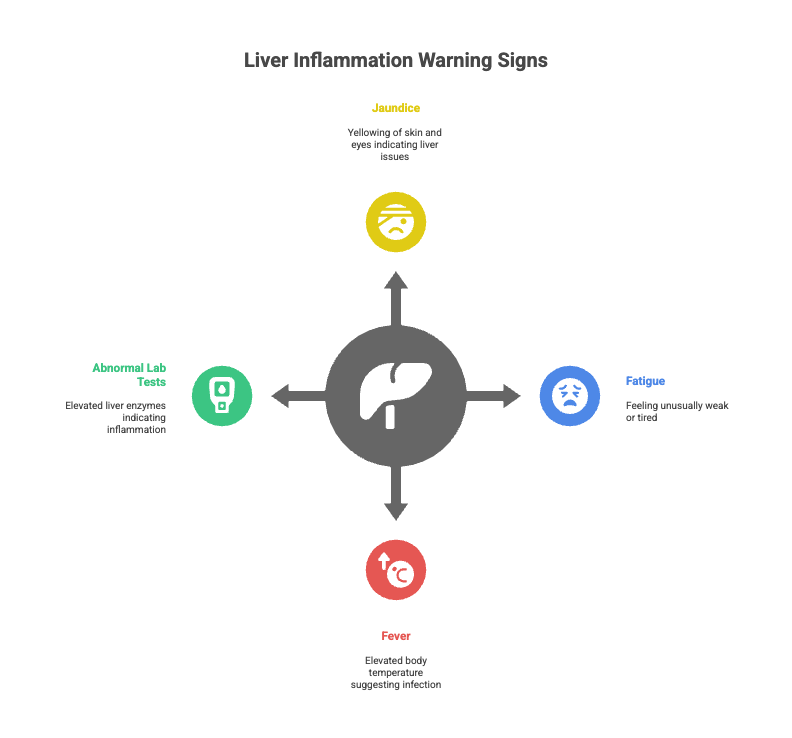
Early detection of Liver Transplant Rejection is key. Warning signs may include:
- Jaundice: Yellowing of skin and eyes.
- Fatigue or malaise: Feeling unusually weak or tired.
- Fever or unexplained illness
- Abnormal lab tests: Elevated liver enzymes (AST, ALT) may indicate inflammation.
Patient analogy: These signs are like warning lights on your car dashboard. If ignored, bigger problems may occur. Regular follow-ups and lab tests help catch rejection early.
Professional / Advanced Section Liver Transplant Rejection
4. Diagnostic Challenges for Liver Transplant Rejection
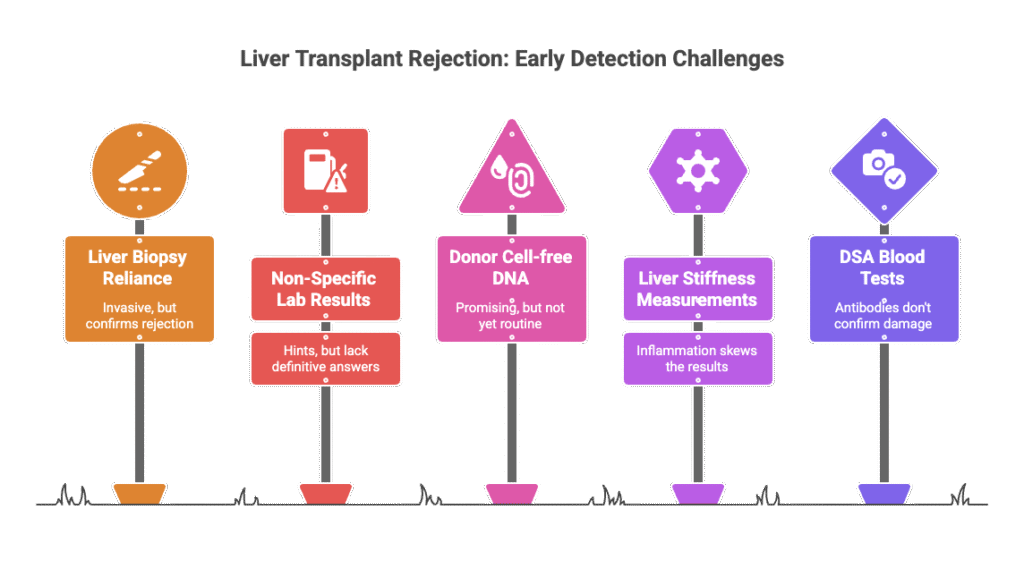
Detecting liver transplant rejection can be tricky because the early warning signs are often subtle.
- Liver biopsy is the gold standard: Think of it like a security inspector checking every corner of your new liver. While blood tests can hint at trouble, only a biopsy can confirm if the immune system is attacking the liver. Doctors strongly discourage giving high-dose steroids without this “inspection,” because treating blindly can sometimes cause more harm.
- Clues from labs: Sometimes, elevated liver enzymes (AST, ALT) or higher eosinophil counts act like warning lights on a dashboard. They tell doctors that the immune system may be overactive, but these signs alone don’t tell the full story.
- Emerging non-invasive tests:
- Donor cell-free DNA: Like a smoke detector in your house, it can detect early “fires” (graft injury) before obvious damage happens. However, it’s still being tested before it becomes routine.
- Liver stiffness measurements (Fibroscan): Imagine checking if a sponge is too stiff. Fibroscan measures liver firmness, which can indicate scarring, but inflammation can make it seem falsely stiff, so the exact cause isn’t clear.
- DSA blood tests: These measure antibodies that may attack the liver. Think of them as security cameras showing potential intruders—but they don’t always confirm if damage is actually happening.
5. T Cell-Mediated Rejection (TCMR) Explained
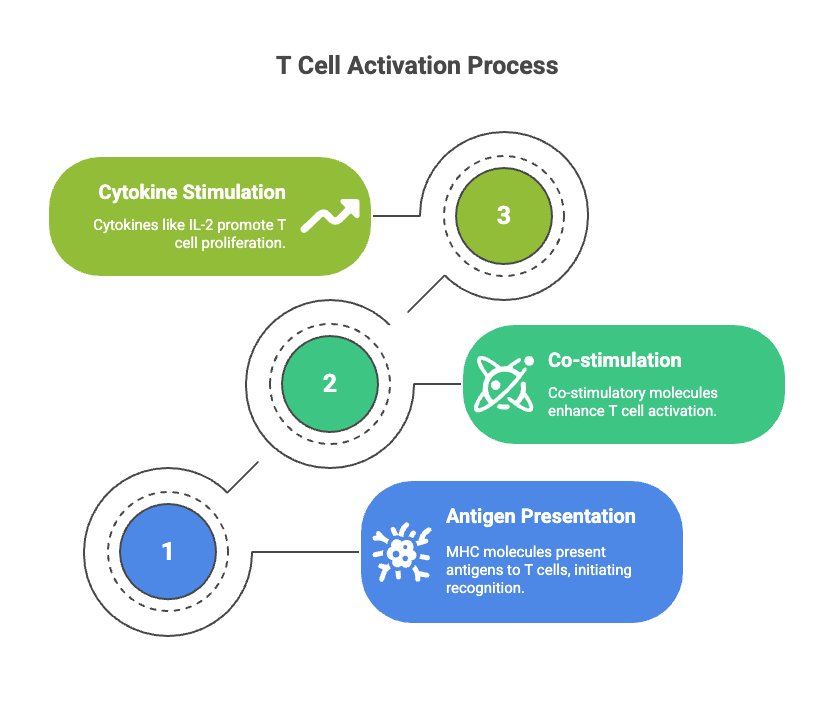
- TCMR occurs when recipient T cells recognise donor MHC antigens.
- Three key signals for T cell activation:
- Signal 1: Antigen presentation (MHC I to CD8+ T cells; MHC II to CD4+ T cells).
- Signal 2: Co-stimulatory molecules (CD28, CD40).
- Signal 3: Cytokines like IL-2 stimulate proliferation.
Professional note: Activated T cells cause hepatocyte injury, portal inflammation, and bile duct damage.
Biopsy scoring follows Banff criteria: mild (<4), moderate (4–6), severe (>7).
6. Antibody-Mediated Rejection (AMR) in Detail

- DSAs (Donor-specific antibodies) bind to HLA on endothelial cells → complement activation → microvascular injury.
- Histology: portal microvascular endothelial hypertrophy, C4d deposition, ductular reaction.
7. Chronic Liver Transplant Rejection: Mechanisms and Management
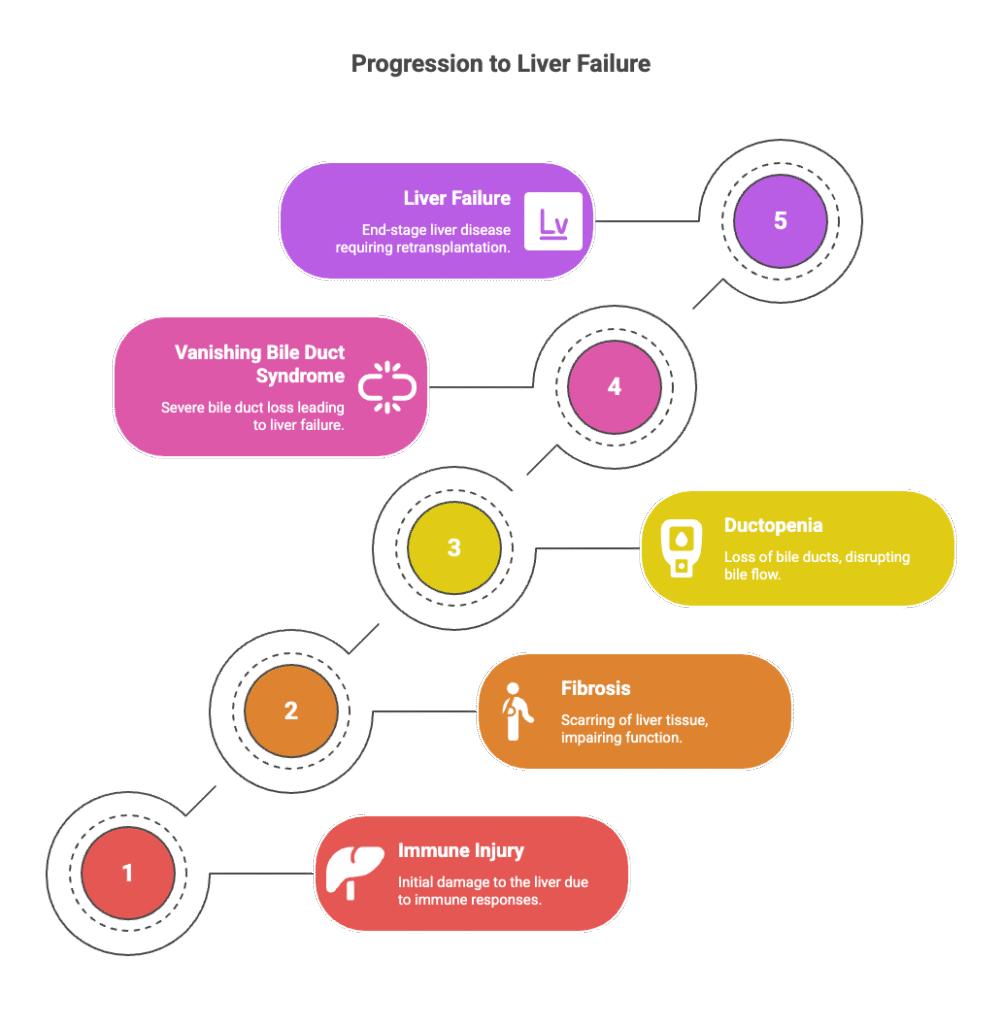
- Long-term immune injury → fibrosis, ductopenia, “vanishing bile duct syndrome.”
Immunosuppressives
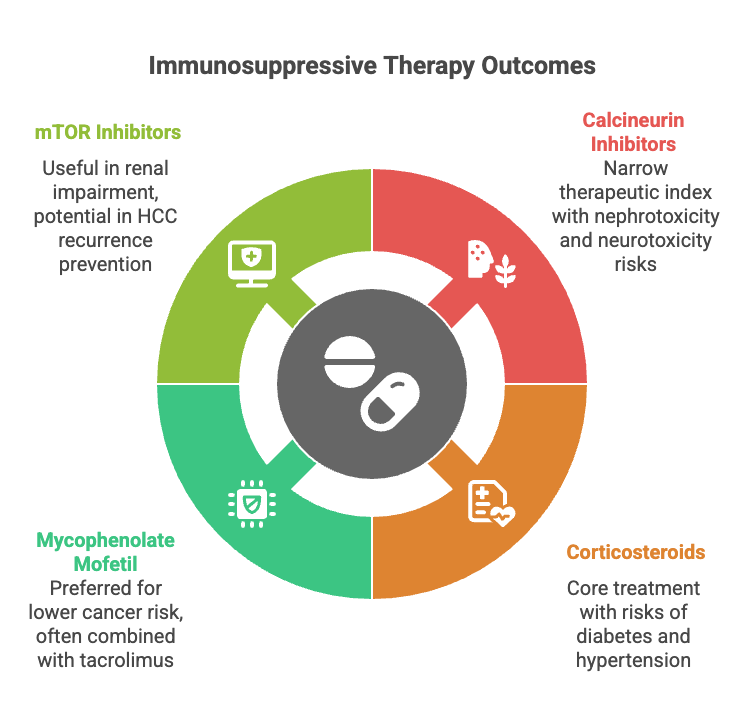
- Calcineurin Inhibitors (Tacrolimus, Cyclosporine)
- Narrow therapeutic index.
- Side effects: nephrotoxicity, neurotoxicity, diabetes, and hypertension.
- Corticosteroids
- Core of most protocols; tapered off in many patients.
- Long-term use is mainly in autoimmune liver disease.
- Risks: diabetes, hypertension.
- Mycophenolate Mofetil (MMF)
- Inhibits lymphocyte proliferation.
- Preferred over azathioprine (lower cancer risk).
- Often combined with low-dose tacrolimus → renal protection.
- Side effects: diarrhoea, bone marrow suppression, and infection.
- mTOR inhibitors (Sirolimus, Everolimus)
- Immunosuppressive + antiproliferative effects.
- Useful in patients with renal impairment.
- Potential role in HCC recurrence prevention (data inconclusive).
Immunosuppressive Treatment of Allograft Rejection

- Mild T Cell-Mediated Rejection (TCMR)
- Intensify CNI dosing.
- Add low-dose prednisone, MMF, or mTOR inhibitors.
- Moderate–Severe TCMR
- IV pulse steroids (methylprednisolone).
- Severe / Resistant TCMR
- Lymphodepleting agents (ATG).
- Risk: infections, PTLD.
- Antibody-Mediated Rejection (AMR)
- No standardised regimen.
- Guided by DSA levels, histology, and graft dysfunction severity.
- First-line: Tacrolimus optimisation + steroid bolus.
- Second-line Treatments Include Plasma exchange, IVIG, and Rituximab.
- Chronic Rejection
- Minimal effective treatment options.
- Retransplantation is definitive management.
8. Immune Checkpoint Inhibitors (ICIs) and Liver Transplant Rejection
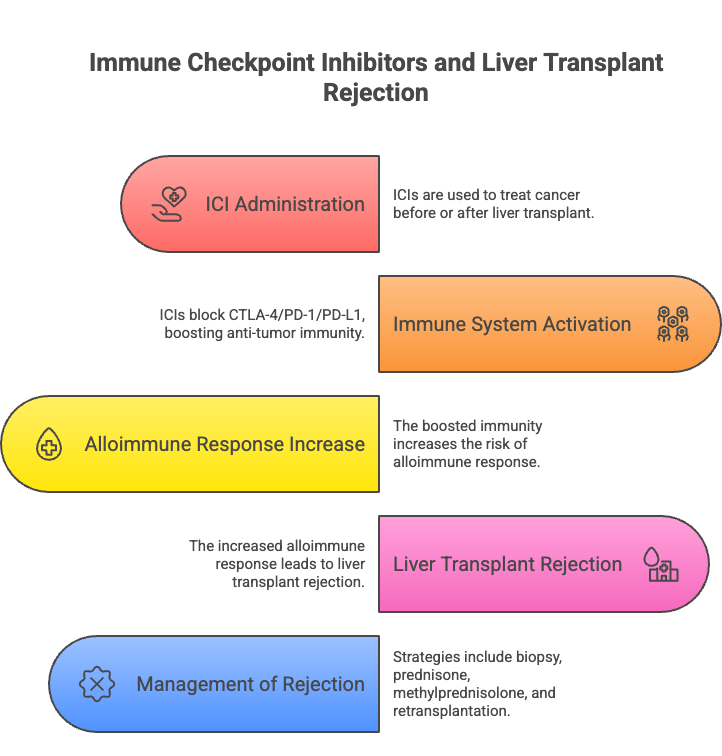
ICI are used to treat cancer before or after a Liver Transplant.
- Mechanism: Block CTLA-4 / PD-1 / PD-L1 → boosts anti-tumour immunity but increases alloimmune response/disrupts immune tolerance for the graft. A minimum 3-month washout time between ICI and LT is recommended.
- Risk: Severe rejection, fatal graft injury; ICI hepatotoxicity is higher in liver allografts.
- Management:
- Grade ≥2 hepatotoxicity → biopsy confirmation.
- Mild: oral prednisone.
- Moderate–severe: IV methylprednisolone.
- Refractory: MMF, CNI reintroduction, ATG, plasmapheresis.
- Salvage retransplantation if graft failure and no oncological contraindications.
🌐 What are CTLA-4, PD-1, and PD-L1?
Think of your immune system like a car:
- The accelerator makes it attack infections or cancer.
- The brakes stop it from overreacting and damaging healthy tissue.
✅ CTLA-4 and PD-1 are like the brake pedals on immune T cells.
✅ PD-L1 is like the signal from other cells telling the brakes to work.
🧩 How they work:
- CTLA-4 (Cytotoxic T-Lymphocyte Antigen-4):
- Found on T cells.
- It tells the T cell to slow down early (like a brake applied at the start of the race).
- PD-1 (Programmed Death-1):
- Also on T cells.
- Works later, during ongoing immune responses, to prevent over-attack.
- PD-L1 (Programmed Death Ligand-1):
- Found on many cells (including cancer cells).
- It binds to PD-1 and says: “Don’t attack me!” → Like a fake ID to escape immune attack.
💊 Immune Checkpoint Inhibitors (ICIs):
- Drugs block CTLA-4, PD-1, or PD-L1.
- This removes the brakes, allowing T cells to attack strongly, which is beneficial for killing cancer.
- But in liver transplant patients, this same effect makes T cells also attack the donor liver, causing rejection.
Frequently Asked Questions: Liver Transplant Rejection
What is the life expectancy of a liver transplant patient?
Most liver transplant recipients live 20 – 30 years or more, depending on their overall health, age, underlying disease, and how well they follow post-transplant care. Modern immunosuppressive medications and close monitoring have greatly improved long-term survival.
Analogy: Think of the new liver as a long-term investment—careful maintenance and regular check-ups help it last for decades.
How do you treat liver transplant rejection?
Treatment depends on the type and severity of rejection:
- Acute T Cell-Mediated Rejection (TCMR): Usually treated by adjusting immunosuppressive medications; steroids may be added for short-term control.
- Antibody-Mediated Rejection (AMR): May require medication adjustments, plasma exchange, or therapies like IVIG or rituximab to remove harmful antibodies.
- Chronic Rejection: Often irreversible; retransplantation may be necessary in severe cases.
Analogy: Treating rejection is like sending extra security guards or shields to protect your liver from “attacking” immune cells.
How to prevent liver transplant rejection?
Key preventive strategies include:
- Consistent use of immunosuppressive medications
- Regular follow-ups and lab monitoring
- Healthy lifestyle: balanced diet, exercise, avoiding infections, and not smoking
- Prompt reporting of unusual symptoms
Analogy: Medications and lifestyle act like traffic signals and security cameras, keeping your liver safe from immune attacks.
How long does organ/liver transplant rejection take?
- Acute rejection: Usually occurs within the first 3 months after transplant
- Late acute or chronic rejection: Can occur months to years later
- Timing varies per patient and depends on adherence to medications and immune system activity.
Analogy: Think of your immune system like a vigilant guard—sometimes it reacts immediately, sometimes months or years later.
What are the first signs of liver transplant rejection?
Early warning signs may include:
- Jaundice (yellowing of skin or eyes)
- Fatigue or unusual weakness
- Fever or unexplained illness
- Abnormal liver function tests (AST, ALT, and bilirubin elevation)
Analogy: These are like warning lights on a car dashboard—catching them early prevents bigger problems.
Can liver transplant rejection be cured?
- Acute rejection: Usually reversible if treated early with medications
- Chronic rejection: Often irreversible; may require a second transplant
Analogy: Acute rejection is like a small fire—it can be put out quickly. Chronic rejection is like rust—once extensive, it may be impossible to reverse.
Can the liver grow again after a transplant?
Yes, the liver has remarkable regenerative ability:
- Partial liver transplants (living donor or split liver) can grow to meet the body’s needs.
- Full liver transplants typically don’t need to grow, but the liver adapts to function fully in the new body.
Analogy: The liver is like a self-repairing sponge—it can regrow to reach the proper size and function.
Can I get a second liver transplant?
Yes, a second or “re-transplant” is possible if the first liver fails due to rejection, disease recurrence, or other complications. Outcomes depend on overall health, timing, and organ availability.
How much liver is needed to regenerate?
- In living donor transplants, at least 30–40% of a donor liver can regenerate in both the donor and the recipient.
- The liver grows rapidly in the first few months post-transplant, often returning to near-normal size.
Analogy: Even a small piece of liver is like a seed—it can grow into a full, healthy organ if properly cared for.
Conclusion: Liver Transplant Rejection
Liver transplant rejection reflects the delicate balance between the liver’s natural tolerance mechanisms and the recipient’s immune response. Early detection, proper medications, and vigilant monitoring are key to long-term success.
Patient takeaway: Understanding warning signs, taking medicines consistently, and maintaining healthy habits can prevent rejection and protect your new liver.
Professional takeaway: Detailed knowledge of immunology helps guide therapy, monitor complications, and optimise long-term outcomes.
🎉 First Consultation with Dr. Tanuja Mallik is FREE!
Get expert advice on liver transplant, recovery, and care — at no cost.
Book your free WhatsApp consultation now:
✅ After booking, please send a WhatsApp message to confirm your slot.
📞 Only first call is free. Follow-ups: ₹499 per session.
