Introduction
Viral Hepatitis – A Silent Epidemic Affecting Millions Worldwide. Numerous viruses can cause viral hepatitis, a common liver infection that has serious health repercussions. Even though it is common, little is known about it, which causes catastrophic liver damage and delayed diagnosis. Having worked as a liver transplant anaesthetist and critical care specialist for years, I have seen how viral hepatitis silently advances to dangerous stages if treatment is delayed. One such story –
🩺 “Late one evening, I got a call about a gasping patient—jaundiced, swollen, crashing fast. pH 6.7. INR unrecordable. Platelets just 10,000. We fought the night and brought him back. Later, we found the trigger: Hepatitis E. Silent. Deadly. Often missed.”
— Dr. Tanuja Mallik, Liver Transplant Anaesthetist
We examine the various forms of viral hepatitis, its modes of transmission, symptoms, complications, preventative techniques, and its worldwide effects in this comprehensive blog, giving you the information you need to safeguard your loved ones and yourself.
What is Viral Hepatitis?
Hepatitis A, B, C, D, and E are the particular viruses that cause viral hepatitis, which is an infection of the liver. During infection, the liver, an essential organ involved in digestion, detoxification, and metabolism, sustains damage that can occasionally be irreparable.
Some forms result in an acute infection that goes away on its own, while others can develop into a chronic condition that raises the risk of malignancy, liver failure, and cirrhosis.
Types of Viral Hepatitis:
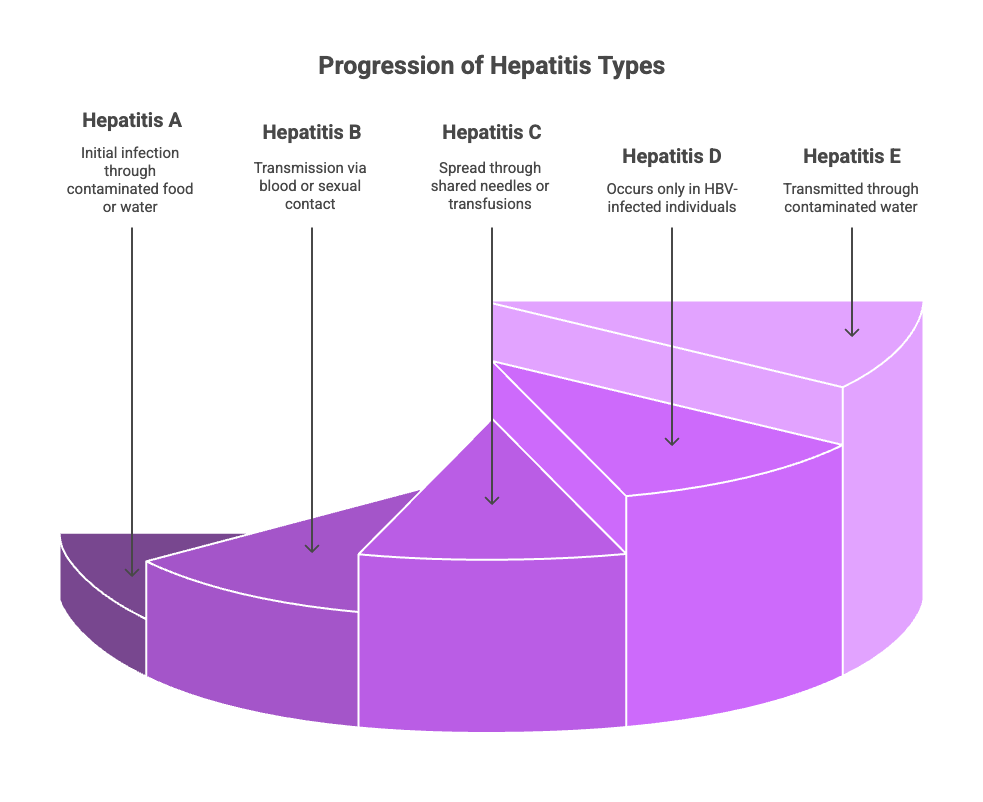
HAV, or hepatitis A
- Transmission: Mainly via ingestion of tainted food or water, via the faecal-oral pathway.
- Time Frame for Incubation: 2–6 weeks.
- Symptoms include fatigue, jaundice, nausea, and abdominal pain.
- Result: Does not result in chronic liver disease; usually resolves on its own with supportive treatment.
- Prevention includes immunisation, good personal cleanliness, clean water, and healthy eating habits.
HBV, or hepatitis B
- Transmission: From mother to kid via pregnancy, sexual contact, and exposure to contaminated blood.
- Six weeks to six months is the incubation period.
- Symptoms: Some people have exhaustion, jaundice, and stomach pain, while many are asymptomatic.
- Chronicity: Five to ten per cent of adults and up to ninety per cent of babies get chronic infections.
- Hepatocellular carcinoma (HCC), liver failure, and cirrhosis are complications.
- Prevention measures include screening blood products, safe sexual practices, and universal vaccination.
HCV, or hepatitis C
- Transmission: By sharing needles, receiving hazardous injections, or receiving transfusions.
- Time Frame for Incubation: 2 weeks to 6 months.
- Until liver disease reaches a late stage, symptoms are frequently absent.
- Chronicity: 70–85% of infections become chronic.
- Liver cancer and cirrhosis are complications.
- Prevention: prevent via safe medical practices
HDV, or hepatitis D
- Transmission: Only occurs in HBV-infected individuals; occurs through sexual contact or blood contact.
- Result: Accelerates liver damage and causes more severe illness.
- Prevention: HDV is avoided via HBV immunisation.
Hepatitis E (HEV)
- Faecal-oral transmission, frequently by tainted water.
- Time Frame for Incubation: 2–10 weeks.
- Similar to HAV, but more severe in pregnant women, are the symptoms.
- Result: Acute; often goes away on its own.
- Prevention measures include better water and sanitation, as well as the availability of vaccines in some nations.
Signs and Symptoms of Viral Hepatitis
Symptoms vary from none (especially in chronic cases) to severe liver inflammation:
- Fatigue and weakness
- Loss of appetite
- Nausea and vomiting
- Jaundice (yellow skin/eyes)
- Dark urine and pale stools
- Abdominal pain, especially upper right quadrant
- Fever and joint pain in some types
Because early symptoms can be subtle or absent, routine screening in high-risk populations is critical.
Complications and Progression
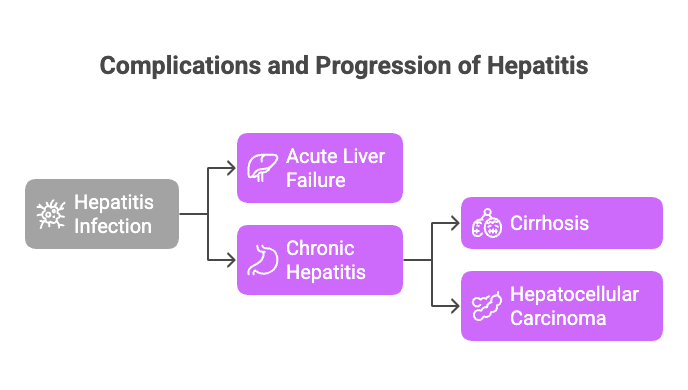
Acute Liver Failure
- A rare yet potentially fatal situation in certain cases of hepatitis.
Cirrhosis and Chronic Hepatitis
- Chronic inflammation impairs liver function by causing scarring.
Hepatocellular carcinoma (HCC)
- Chronic HBV and HCV infections significantly increase the risk of liver cancer.
Extrahepatic Manifestations
- Certain hepatitis viruses induce autoimmune diseases and damage the kidneys, skin, and joints.
Global Epidemiology:
According to the WHO and CDC:
- HBV: 296 million chronic infections worldwide, with ~820,000 deaths annually.
- HCV: 58 million chronic infections, ~290,000 deaths annually.
- HAV and HEV: Cause millions of acute infections yearly, especially in low sanitation areas.
- Highest prevalence in Asia and Africa, but cases are rising globally due to migration and risky behaviours.
Viral Hepatitis as a Communicable Disease
Because it can be transmitted through certain routes, such as faecal-oral, blood-borne, or sexual contact, viral hepatitis is categorised as a communicable disease. The communicability of each category varies:
The faecal-oral pathway is the main way that hepatitis A and E are spread, and it is frequently connected to tainted food, water, and inadequate sanitation. Outbreaks may result from these viruses, particularly in places with subpar water and sewage systems.
Because hepatitis B, C, and D are spread by blood and bodily fluids, they are serious risks in medical facilities, among intravenous drug users, and through risky sexual behaviour.
Since many infected people do not exhibit any symptoms for extended periods, viral hepatitis infections can spread silently, which is why the disease is frequently referred to as a “silent epidemic.”This feature makes public health surveillance and early detection essential to breaking chains of transmission.
Surveillance Strategies for Viral Hepatitis
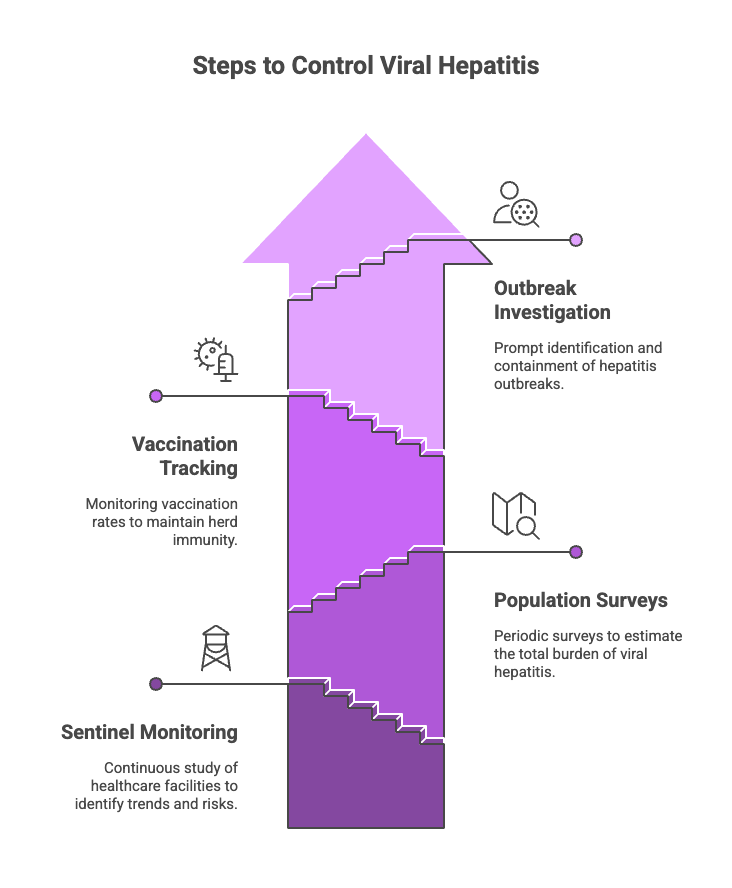
The foundation of worldwide viral hepatitis control is efficient surveillance. Monitoring disease patterns, identifying outbreaks, and assessing the success of preventative initiatives are all made easier by surveillance. It consists of:
- Notification and Reporting of Cases
Public health authorities must be notified by healthcare practitioners of confirmed cases of viral hepatitis. Rapid resource allocation and public health responses are made possible by this real-time reporting. Hepatitis B and C are now considered nationally notifiable illnesses in many nations.
- Monitoring in the Lab
Frequent laboratory testing and confirmation of viral hepatitis cases aid in monitoring infection rates and identifying certain virus genotypes and mutations, which are essential for developing vaccines and treatment plans.
- Monitoring by Sentinels
To offer comprehensive information on incidence, prevalence, and risk factors, a subset of healthcare facilities or populations is continually studied. This aids in identifying high-risk populations or new trends, directing focused responses.
- Surveys based on populations
The total burden of viral hepatitis in the population, including instances that go undetected, is estimated by periodic seroprevalence surveys. Vaccination plans and public health policies are informed by these surveys.
- Tracking Vaccination Coverage
Monitoring vaccination uptake rates for hepatitis A and B is essential for maintaining herd immunity and avoiding new infections, particularly in susceptible groups like newborns and medical personnel.
- Outbreak Investigation
Hepatitis outbreaks must be promptly identified and contained. Public health teams carry out control measures, such as mass vaccination and awareness campaigns, and look into the causes and mechanisms of transmission.
The Role of Surveillance in India and Globally
In India’s national programs, hepatitis surveillance is incorporated into broader frameworks for communicable illnesses, emphasising:
- Strengthening lab networks to facilitate timely diagnosis.
- Increasing the coverage of vaccinations under the Universal Immunisation Program (UIP).
- Enhancing programs for public education on transmission and prevention.
WHO’s Global Hepatitis Programme sets ambitious goals to eradicate viral hepatitis as a public health concern by 2030, primarily through the use of efficient monitoring tools to track progress.
Prevention: The Most Effective Weapon Against Viral Hepatitis
Immunisation
- There are safe and efficient vaccinations for HAV and HBV.
- WHO advises that all infants be vaccinated against HBV.
- There are currently no commonly used vaccinations for HDV and HCV (indirectly avoided).
Safe Procedures
- Consistently use condoms.
- Don’t share razors, needles, or other personal objects that could come into contact with blood.
- Make sure sterilised equipment is used for medical procedures.
Hygiene
- Hands should always be completely cleaned before handling or preparing food.
- Sip boiled or treated water.
- Keep food preparation hygienic.
Diagnosing Viral Hepatitis
Diagnosis involves:
- Blood tests detecting viral antigens/antibodies and liver enzymes (ALT, AST).
- FIB-4 Index scoring to assess advanced fibrosis
- PCR testing for viral load.
- Imaging (ultrasound, elastography, CT scan) for liver damage.
- Liver biopsy in select cases.
FIB-4 Index in Hepatitis:
📊 FIB-4 Index Calculator
Enter the values below to calculate the FIB-4 index for liver fibrosis.
Note: for interpretation and to know more about the FIB-4 index, check this link>>https://livertransplanthelp.com/fib-4-index-calculator/
The FIB-4 index was originally developed to assess liver fibrosis in patients with HIV and Hepatitis C co-infection, particularly to evaluate the risk of advanced cirrhosis. This scoring system has demonstrated high negative predictive value (NPV), meaning that individuals with a low FIB-4 score (<1.3) are highly unlikely to have advanced liver fibrosis or cirrhosis. As a result, a low score can effectively rule out severe liver disease. On the other hand, a higher score, especially above 2.7, carries significant positive predictive value (PPV), indicating a higher likelihood of advanced fibrosis or cirrhosis.
In the community setting, the FIB-4 index is of great significance. For individuals with a score of less than 1.3 and no metabolic risk factors like diabetes, hypertension, or dyslipidemia, monitoring every 2 to 3 years may be sufficient. However, for individuals with a score of less than 1.3 but with metabolic risk factors, more frequent monitoring (every 1 to 2 years) is recommended to track any potential progression. This makes the FIB-4 index a useful tool in assessing the progression of liver damage in Hepatitis patients and guiding clinical management, especially for those at risk of developing advanced liver disease.
Treatment and Management Strategies
Hepatitis A and E
- No specific antiviral treatment.
- Supportive care: rest, hydration, nutrition.
Hepatitis B
- Antiviral drugs (e.g., tenofovir, entecavir) suppress viral replication.
- Regular monitoring to assess liver damage and cancer risk.
- Some patients may require lifelong therapy.
Hepatitis C
- Direct-acting antivirals (DAAs) cure >95% of cases within 8–12 weeks.
- Treatment personalised based on genotype and fibrosis stage.
Hepatitis D
- Difficult to treat; interferon therapy has limited success.
- Prevention through HBV vaccination remains key.
Lifestyle changes
- Avoid alcohol and hepatotoxic drugs.
- Maintain a balanced diet and healthy weight.
- Regular medical follow-up for liver function and screening for cancer.
- Psychological support and counselling can improve quality of life.
Safe Sex and Hygiene:
- Consistent condom use reduces HBV and HCV transmission risk.
- Avoid multiple sexual partners.
- Educate communities about transmission routes and stigma.
- Promote hand hygiene and safe food/water practices.
Future Directions: Vaccines and New Therapies
- Research is ongoing for HCV vaccines.
- Novel antivirals and immunotherapies are in development.
- Public health efforts focus on elimination goals by 2030 (WHO).
Conclusion: Viral Hepatitis is Preventable and Manageable with Awareness and Action
Viral hepatitis is a global health challenge with serious consequences. However, through vaccination, safe practices, early diagnosis, and modern treatments, we can drastically reduce its burden.
Be proactive—get vaccinated, practice safe hygiene, seek regular screenings, and spread awareness. Together, we can save millions of lives.
Frequently Asked Questions
What is viral hepatitis, and why is it a significant global health issue?
Viral hepatitis is an inflammation of the liver caused by specific viruses: Hepatitis A, B, C, D, and E. The liver is a crucial organ, and damage from these infections can be severe, sometimes irreversible. While some types cause short-term illness, others become chronic, increasing the risk of serious conditions like cirrhosis, liver failure, and liver cancer. It's considered a global health challenge because millions worldwide are affected, often silently, leading to late diagnosis and severe complications. The World Health Organisation (WHO) and the CDC report hundreds of millions of chronic infections globally, resulting in significant annual deaths.
How are the different types of viral hepatitis transmitted?
The transmission routes vary depending on the specific hepatitis virus:
- Hepatitis A (HAV) and Hepatitis E (HEV) are primarily spread through the faecal-oral route, meaning through contaminated food or water, often due to poor sanitation.
- Hepatitis B (HBV), Hepatitis C (HCV), and Hepatitis D (HDV) are transmitted through exposure to infected blood or body fluids. This includes sexual contact, sharing needles or other sharp items, transfusions of unscreened blood, and perinatal transmission from mother to child (HBV). Hepatitis D specifically only occurs in people who are already infected with Hepatitis B.
What are the common signs and symptoms of viral hepatitis, and why is early detection often difficult?
Symptoms of viral hepatitis can range from none at all, especially in chronic cases, to severe signs of liver inflammation. Common symptoms include fatigue, weakness, loss of appetite, nausea, vomiting, jaundice (yellowing of skin and eyes), dark urine, pale stools, and abdominal pain (particularly in the upper right side). Fever and joint pain can also occur with some types. Early detection is often difficult because many infected individuals, especially with chronic types like HBV and HCV, can be asymptomatic for long periods. This "silent epidemic" nature makes routine screening and surveillance critical for identifying cases before significant liver damage occurs.
What are the potential complications of viral hepatitis, particularly the chronic types?
Chronic viral hepatitis infections, primarily Hepatitis B and C, can lead to several serious complications. Persistent liver inflammation can cause scarring (fibrosis), which progresses to cirrhosis, a condition where the liver is severely damaged and its function is impaired. Cirrhosis significantly increases the risk of developing hepatocellular carcinoma (HCC), a type of liver cancer. In rare cases, viral hepatitis can also lead to acute liver failure, a life-threatening emergency. Additionally, some hepatitis viruses can affect other organs, causing extrahepatic manifestations involving the kidneys, skin, joints, and potentially triggering autoimmune conditions.
How can viral hepatitis be prevented?
Prevention strategies for viral hepatitis include several key approaches:
- Vaccination: Safe and effective vaccines are available for Hepatitis A and Hepatitis B. Universal infant HBV vaccination is recommended by the WHO. While there's no widely used vaccine for HCV, HBV vaccination indirectly prevents HDV infection.
- Safe Practices: Avoiding sharing needles, syringes, razors, or any items that may come into contact with blood is crucial for preventing HBV and HCV. Practising safe sex using condoms consistently can reduce the risk of HBV and HCV transmission. Ensuring medical procedures are performed with sterile equipment is also vital.
- Hygiene: Practising good hand hygiene, especially washing hands thoroughly with soap and water before eating or preparing food, is essential for preventing HAV and HEV. Drinking treated or boiled water and maintaining sanitary food preparation practices also help.
How is viral hepatitis diagnosed?
Diagnosing viral hepatitis typically involves several steps:
- Blood tests are the primary method, detecting viral antigens or antibodies specific to each hepatitis virus. These tests also measure liver enzymes like ALT and AST, which can indicate liver damage.
- PCR testing (polymerase chain reaction) is used to detect the presence of the virus itself and measure the viral load, which is particularly important for managing chronic infections and monitoring treatment effectiveness.
- Imaging techniques such as ultrasound and elastography can assess the extent of liver damage, including fibrosis or cirrhosis.
- In select cases, a liver biopsy may be performed to examine liver tissue directly and assess the severity of inflammation and scarring.
What are the treatment options for the different types of viral hepatitis?
Treatment approaches vary depending on the specific hepatitis virus:
- For Hepatitis A and E, there is typically no specific antiviral treatment. Management focuses on supportive care, including rest, hydration, and maintaining good nutrition, as these infections usually resolve on their own.
- For Hepatitis B, antiviral medications like tenofovir and entecavir are used to suppress viral replication. Treatment may be lifelong for some patients and requires regular monitoring to assess liver health and screen for liver cancer.
- For Hepatitis C, direct-acting antivirals (DAAs) have revolutionised treatment, curing over 95% of cases within 8-12 weeks. Treatment is personalised based on the specific genotype of the virus and the stage of liver fibrosis.
- Hepatitis D is difficult to treat, with limited success from interferon therapy. Prevention through HBV vaccination remains the key strategy.
How does surveillance play a role in controlling viral hepatitis globally?
Effective surveillance is crucial for controlling viral hepatitis worldwide. Surveillance systems help monitor disease trends, detect outbreaks, and evaluate the effectiveness of prevention programs. Key strategies include mandatory case reporting by healthcare providers to public health authorities, laboratory surveillance to confirm cases and track virus types, sentinel surveillance in specific populations to identify trends, population-based surveys to estimate the overall burden of infection (including undiagnosed cases), monitoring vaccination coverage rates, and rapid investigation of outbreaks. Robust surveillance allows for targeted interventions, resource allocation, and tracking progress towards global elimination goals set by organisations like the WHO.
🧠 Resources to Help You Prepare, Act & Recover
-
👩⚕️ 1:1 Consultations:
Get expert guidance on liver failure and poisoning-related emergencies -
📥 Download:
Know Your Medicine (KYM) – Free eBook for liver protection & awareness -
📘 Deep Dive Guide:
Liver Transplant Made Simple – eBook & Paperback -
🧰 Recovery Resource Kit:
Complete tools, supplements & mental support for transplant healing